The annual meeting of the European Association for the Study of Diabetes (EASD) was held in Madrid, Spain, from September 9 through 11. The event was attended by researchers, clinicians, pharmaceutical and device companies, regulators and leaders in the diabetes field from more than 120 countries, including experts from Breakthrough T1D. The meeting showcased numerous studies presented by Breakthrough T1D-funded researchers whose work focuses on curing type 1 diabetes (T1D) and improving the lives of individuals living with the disease. The research presented at EASD covered Breakthrough T1D’s entire research portfolio, encompassing disease-modifying therapies, cell therapies, and complications.
Here are a few EASD highlights.
Cell therapy update
A session at EASD hosted by Vertex explored the promise of cell therapies. This session, which featured several longtime collaborators funded by Breakthrough T1D, including Stephanie Amiel and Jennifer Sherr, took a look at where T1D management is today, barriers to people doing better, and how cell therapies can potentially transform treatment and management of this disease—including, most importantly, better outcomes. Some notable takeaways:
- People with T1D are still experiencing severe hypoglycemia and are unable to meet glycemic targets—even though the tools, including continuous glucose monitoring and automated insulin delivery systems—are vastly improved. Cadaveric islet transplants (from deceased donors) can restore insulin production in people with T1D, but they will never be a scalable solution for the T1D community due to a lack of supply of cells and the downsides to the accompanying immunosuppression. However, this benefit risk profile is favorable for certain people.
- Stem cell-derived islets are working in clinical trials with the use of immune suppression—a critical step. The next step is to continue to follow these trials and work to develop ways to keep the cells safe without the use of immunosuppression.
Dr. Piotr Witkowski, a longtime Breakthrough T1D collaborator and funded researcher, presented interim data from Sernova’s Cell Pouch Phase I/II trial. Key findings include:
- Long-Term Islet Function: Over five years, the Cell Pouch continued to show well-vascularized and functioning islets that were producing insulin.
- Safety and Retrievability: After five years, the Cell Pouch showed no signs of harmful fibrotic tissue or degradation.
- Patient Outcomes: All six patients in the trial’s initial cohort achieved sustained insulin therapy independence with the use of immune suppression.
- Future Steps: The trial will continue with an optimized immune suppression regimen.
Dr. Trevor Reichman also gave a much-anticipated update on VX-880—Vertex’s stem cell-derived islet therapy. (As a reminder, this therapy derives from the work of Doug Melton, who was supported by Breakthrough T1D-funded and T1D Fund). Vertex has been providing regular updates on this study, and there is more good news since the last update at ADA this summer. Of note:
- All participants who received the full dose are showing benefits, including:
- Insulin production as measured by C-peptide
- Elimination of severe hypoglycemia
- Significantly improved glucose control, with HbA1c’s less that 7% and >70% time in range.
- All 4 participants who received the full dose of cells with a follow-up after more than one year met the primary endpoint of eliminating severe hypoglycemic events and achieved the secondary endpoint of insulin independence.
- The safety profile is consistent with the immunosuppressive regimen, infusion procedure, and complications of longstanding T1D.
- The study has been expanded to enroll 37 participants.
Key takeaway: This session at EASD showed why Breakthrough T1D is doubling down on cell therapies as cures for T1D and is working to ensure there is a regulatory pathway. Thanks to decades of work and funding, stem cell-derived therapies, like the ones being used by Vertex (and developed with funding from Breakthrough T1D), have the upside of virtually eliminating disease burden. We will continue to focus on them until they are a reality.
T1D and cardiovascular disease
On Tuesday, September 10, Breakthrough T1D staff was in the room for an EASD update on cardiovascular disease and T1D. These presentations highlighted the urgent need to diagnose and address this chronic condition.
- In a study presented by Michal Dubsky, individuals with T1D without a previous history or signs of cardiovascular disease without previous history or signs of cardiovascular disease with high calcium score and carotid plaque (indicators of cardiovascular disease) should be considered very high risk. This was discovered using a non-invasive imaging technique called optical coherence tomography.
- A study presented by Patrik Smidtslund showed that people with T1D are at a higher risk of myocardial infarctions, or heart attacks—in particular, non-ST-elevation myocardial infarctions. Diabetic kidney disease and retinopathy were associated with increased myocardial infarction risk.
- Roberta Lupoli presented data showing that poorer vascular function is linked to increased time above range—and that three months on automated insulin delivery (AID) systems lower time above range and improve endothelial function (the cells that line blood vessels and the heart).
The recent results of Bayer’s FINEARTS-HF study, a pivotal trial to evaluate the efficacy and safety of the oral medication finerenone for heart failure, were discussed. Finerenone showed statistically significant improvement in cardiovascular outcomes in adults with heart failure. The trial recruited participants with heart failure regardless of diabetes status or type. Finerenone (AKA Kerendia) is currently approved for kidney disease in T2D and is under investigation for kidney disease in T1D.
This is welcome news for a few reasons. First off, more drugs are needed for people with cardiovascular disease and T1D. Secondly—finerenone is approved in the US for use in reducing the risk of cardiovascular disease and kidney disease in type 2 diabetes—not T1D. The inclusion of people with T1D in this trial is significant. Breakthrough T1D is actively working to assess the potential benefit in T1D through clinical trials by supporting Bayer’s FINE-ONE study, which is using finerenone to treat kidney disease in people with T1D.
Key takeaway: Cardiovascular disease is a significant challenge for the T1D population, and we need to develop better interventions specifically for people with T1D. Some of the best tools to address cardiovascular disease, including SGLT inhibitors, are not approved for use in T1D—which is something Breakthrough T1D is committed to changing.
Do devices help people with T1D?
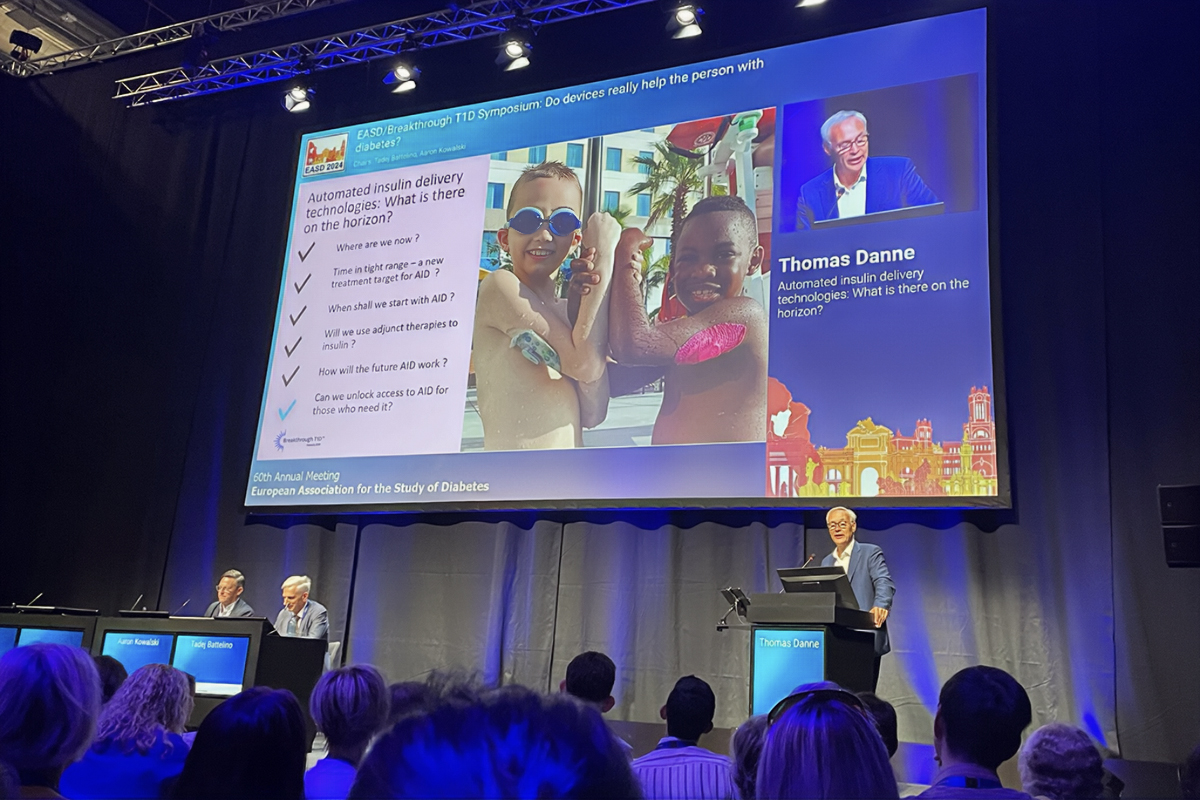
A standing-room-only symposium at EASD chaired by Breakthrough T1D CEO Aaron Kowalski, Ph.D., featuring Breakthrough T1D Chief Medical Officer, International, Thomas Danne, M.D., tackled whether or not people are doing better with the myriad tools available today.
- Lutz Heinemann discussed Connected Smart Pens (CSPs). These devices are closing a critical gap between people who do not want to wear a pump, but benefits are not entirely straightforward and vary depending on the user and the device.
- Mark Evans explored the risks of connected devices. On the plus side, it gives more people access to data—and there is significantly more data available. This can be accompanied by increased anxiety, nagging, etc. Additionally, there are cybersecurity risks as well as the fact that not everyone has access to the technology required to connect devices.
- Lastly, Dr. Thomas Danne discussed the transformative nature of AID systems, (which Breakthrough T1D, Dr. Danne, and Dr. Kowalski played a significant role in developing). These systems are still underutilized worldwide for a variety of reasons. However, diabetes technology is not a cure now, and it will not be in the future. Disease-modifying and cell therapies are going to be the advances that allow us to walk away from this disease for good.
- Dr. Danne also discussed how continuous ketone monitoring can make SGLT use safe in people with T1D, the importance of interoperability between AID systems, and transitioning to using tight time-in-range (70-140 mg/dl) as the key measure of glycemic control. These are all priorities of Breakthrough T1D that Dr. Danne is working toward.
Key takeaway: New tech has been transformational—and it will continue to get better—but more people need access to it, and earlier. Diabetes technology will not cure this disease. It does have the potential to keep people healthy so they can take advantage of cures when they are realized.
Coming Soon: ISPAD
Following EASD, the next big meeting on the T1D calendar is the International Society for Pediatric and Adolescent Diabetes (ISPAD)’s annual meeting from October 16 through 19 in Lisbon, Portugal. We’ll provide the highlights next month.