Type 1 diabetes (T1D) doesn’t discriminate. It affects people of all races, ethnicities, ages, and socioeconomic backgrounds. Although its exact causes are unknown, researchers have uncovered type 1 diabetes risk factors that increase a person’s likelihood of developing the condition.
Family history
Having a family history of type 1 diabetes is the highest risk factor for developing the disease—a first-degree relative (parent, sibling, or child) with T1D increases your risk up to 15-fold. However, nearly 85% of diagnoses occur in people who have no family members with the disease.
Breakthrough T1D-funded researchers have tracked data from nearly 8,000 high-risk children to estimate future risk for T1D more precisely in The Environmental Determinants of Diabetes in the Young (TEDDY) study. A family follow-up to this study focuses on screening and monitoring siblings and parents of TEDDY participants, who have an increased genetic risk for T1D. The goal is to enhance early detection and prevention programs, better understand the natural progression of T1D, and potentially identify new genetic markers that can help predict the risk of T1D development.
Early Detection
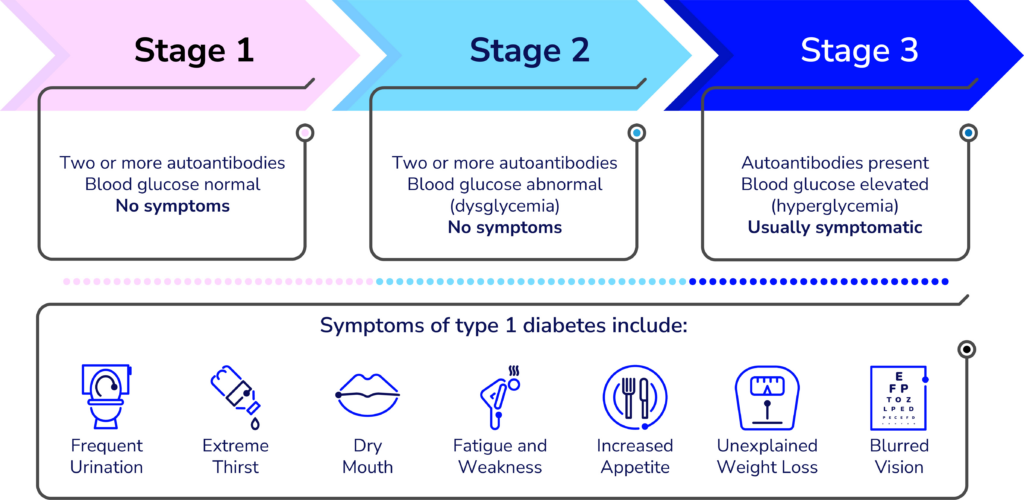
Thanks to advances in research and a better understanding of the human immune system, we are now able to identify a person’s risk for T1D many years before the onset of symptoms through a simple blood test. Screening can reduce the risk of complications at diagnosis and also help researchers better identify who is at risk. This leads to the development of disease-modifying therapies that can slow, halt, or reverse the progression of T1D.
Age
A person’s age is a type 1 diabetes risk factor. While people can experience the onset of T1D at any age, many are diagnosed in early elementary school or as preteens, with ages 10-14 having the highest occurrence of diagnoses.
Environmental triggers
Research has not found a definite environmental trigger for type 1 diabetes. Viruses and exposure to gluten, cow’s milk, antibiotics, and more have all been extensively studied, yet no certain links have been made. “The evidence has not been conclusive,” says Laura Jacobsen, M.D., Assistant Professor and Pediatric Endocrinologist at the University of Florida. “It may be because there are multiple or different triggers for different subsets of the population.”
Ethnic and geographic triggers
The risk for type 1 diabetes has historically been highest in those with white European ancestry. However, the diversity of the population with T1D is increasing, meaning the risk is going up in minority populations. Research is ongoing in this area to address this increasingly global problem. Visit the T1D Index for a detailed look at type 1 diabetes prevalence around the world.
Geographically, there are countries where the risk of T1D is higher than others, but “ultimately it is underlying genetics that impact risk,” Dr. Jacobsen said.
Researchers are still trying to understand how and why genes and environment are T1D risk factors. Breakthrough T1D continues to fund this research so that, one day, we will be able to prevent, reverse, and cure type 1 diabetes.
ADA Recap Series
This article is the second of our three-part ADA Recap Series. Breakthrough T1D was on site in Chicago, IL from June 20-23 for the American Diabetes Association’s (ADA) 85th Scientific Sessions. We’re here to report on the latest-and-greatest type 1 diabetes (T1D) advancements—including many driven by Breakthrough T1D funding. Look out for tomorrow’s article for updates on Medical Affairs.
Cures
Breakthrough T1D’s Cures program focuses on early detection, disease-modifying therapies, and cell therapies with the goal of working toward effective cures for T1D.
Cell therapies were front-and-center at ADA 2025. We have some exciting clinical trial updates and new ideas for optimizing islet transplantation.
Cell therapies
Autologous cell transplantation
Autologous cells are those removed from an individual and implanted back into the same individual. These cells can be modified in a laboratory before implantation. Autologous cells are still susceptible to autoimmunity in T1D, so cell protection strategies (gene-editing, encapsulation, immune modulation, etc.) are expected to be required.
Allogenic cell transplantation
Allogenic cells are those that are derived from a source other than the recipient, such as deceased donors or precursor-derived manufactured cells. Allogenic cell transplants require immunosuppression because they stimulate an immune response. Breakthrough T1D’s Cell Therapies program is focused on allogenic cells—specifically manufactured cells—because they can be generated at large scale.
One-year updates on Vertex’s manufactured cell therapy, zimislecel
- Presenter: Michael Rickels, M.D. (University of Pennsylvania)
- Zimislecel (VX-880) is a manufactured islet therapy that requires immunosuppression, infused into a vein in the liver in people with T1D who have impaired hypoglycemic awareness and severe hypoglycemic events.
- The phase 1/2 clinical trial, which is part of the pivotal phase 1/2/3 FORWARD-101 trial, is complete. Twelve participants received a single infusion of a full dose of cells and were followed for at least one year.
- All 12 participants achieved the primary endpoint, which was elimination of severe hypoglycemic events and HbA1c levels less than 7%. 10/12 (83%) participants are insulin independent.
- All 12 participants demonstrated sustained insulin production as measured by C-peptide, reduced external insulin therapy use, and achieved greater than 70% time in range.
- There were no serious adverse events. Mild to moderate adverse events were consistent with the immunosuppression regimen, infusion procedure, and complications from T1D.
- These data were published in the New England Journal of Medicine and represent further evidence of the curative potential of manufactured islet transplantation for T1D.
- Breakthrough T1D’s support for Doug Melton, Ph.D.—whose proprietary lab-created beta cells are now being advanced by Vertex—goes back decades, both via research grants and an investment from the T1D Fund: A Breakthrough T1D Venture.
6-month update on Sana Biotechnology’s immune-evasive islets
- Presenter: Per-Ola Carlsson, M.D., Ph.D. (Uppsala University)
- Sana’s donor-derived islet therapy engineered with Hypoimmune (HIP) technology can evade the immune system without immunosuppression.
- These cells were implanted intramuscularly in a first-in-human study into a person with T1D with no measurable insulin production.
- Six months post-transplant, this person is consistently making their own insulin, as measured by C-peptide levels. Yet, they still require external insulin therapy because they received a smaller dose of cells than the dose that would be required to achieve insulin independence. They did not experience any serious side effects, so the cells and procedure are safe and well-tolerated.
- A Mixed Meal Tolerance Test (MMTT) confirmed that these cells are not only surviving but also responding to changes in blood glucose levels.
- This is a promising first step toward a functional cure for T1D that does not require immunosuppression. Sana Biotechnology is planning on applying this technology to manufactured islets.
- Sana has received support from the T1D Fund to advance their HIP technology in islets, and Breakthrough T1D continues to work closely with them.
A new transplantation site for autologous manufactured islets
- Presenter: Hongkui Deng, M.D. (Peking University)
- Cells derived from adipose tissue (fat) can be removed from a person and chemically induced in the laboratory to become islet cells.
- Implantation of autologous manufactured islets into the sub-anterior rectus sheath in preclinical models of T1D improves glycemic control.
- In humans, this implantation site is easily accessible by an ultrasound-guided needle.
- In a first-in-human study, autologous manufactured islets were implanted into this site in a person with T1D. This person no longer needs external insulin therapy and has greatly improved blood glucose control. This person had also received a liver transplant and was taking immunosuppressants.
A new encapsulation device for immune protection of transplanted islets
- Presenter: Nicolas Laurent, Ph.D. (Adocia)
- Adoshell® is a novel islet cell encapsulation device that can shield islets from the immune system, meaning that immunosuppressants are not needed.
- The hydrogel-based device is non-degradable, easily retrievable, and allows the exchange of glucose and insulin from the vasculature surrounding the device while excluding immune cells from encapsulated islets based on pore size.
- This device showed promise in animal models, and human clinical testing is next.

Cell therapies highlight: Breakthrough T1D-funded research
Tom Bollenbach, Ph.D. (Advanced Regenerative Manufacturing Institute; ARMI) presented on challenges and solutions for large-scale manufacturing of islet cells. The goal is to generate scalable, automated manufactured islets that can be used by labs around the world to accelerate research progress using a unique, validated, and reliable cell source. Some challenges include ensuring the manufactured cells can survive shipment from the facility to research labs and maintain their insulin-producing capacity when they are used in different labs. ARMI is working with the Beta Cell Replacement Consortium to address these challenges.
Antonio Citro, Ph.D. (San Raffaele Hospital) presented his work on ensuring that transplanted islets have enough oxygen and nutrients (“vascularization”) to survive and function. Dr. Citro described an approach tested in animal models referred to as “natural scaffolds” in which all cells are removed from a donor organ, such as a lung, leaving behind blood vessel structures and other structural components. Islet cells can be injected and grafted onto this scaffold to create a mini organ of islet cells, which can then be tested for functionality before and after implantation.
Andrew Pepper, Ph.D. (University of Alberta) also presented vascularization strategies to increase the survival and functionality of transplanted islets. The implantation of a biomaterial under the skin will trigger the immune system and initiate a foreign body reaction, which results in the formation of blood vessels and structural components around the foreign object. Removal of the object leaves a hollow pre-vascularized core suitable for islet transplantation. This process can be optimized by using a biodegradable material, so no removal is required, and by the addition of “accessory cells” that help maintain a vascularized environment for islets.
Key takeaways
Cell therapies are making significant headway in clinical trials, and people receiving manufactured cells are becoming insulin independent. Researchers are tackling the biggest challenges for optimizing islet transplantation, including large-scale manufacturing, ensuring cell survival, and preventing detection by the immune system.
Disease-modifying therapies
A major focus at ADA 2025 was addressing the underlying immune mechanisms of T1D—including alterations in immune cells that facilitate beta cell destruction and other factors that contribute to autoimmunity onset. Read on for some highlights.
The role of B cells in T1D autoimmunity
- Presenter: Mia Smith, Ph.D., DVM (University of Colorado)
- B cells are a type of immune cell that can activate destructive immune cells that facilitate autoimmunity in T1D.
- B cells can become wrongly activated against insulin-producing beta cells due to converging dysregulation of factors that regulate immunity.
- These cells represent another potential target for disease-modifying therapies in T1D.
Disease-modifying therapies highlight: Breakthrough T1D-funded research
Emrah Altindis, Ph.D. (Boston College) presented on the role of the gut microbiome in T1D. His studies found that people with T1D tend to have more inflammatory bacteria in their gut microbiome. Dr. Altindis and his team identified a particular bacterial population that can enhance T1D onset in animal models due to changes in immune cells that contribute to T1D autoimmunity. These studies provide insight into additional factors that can drive immune changes in T1D.
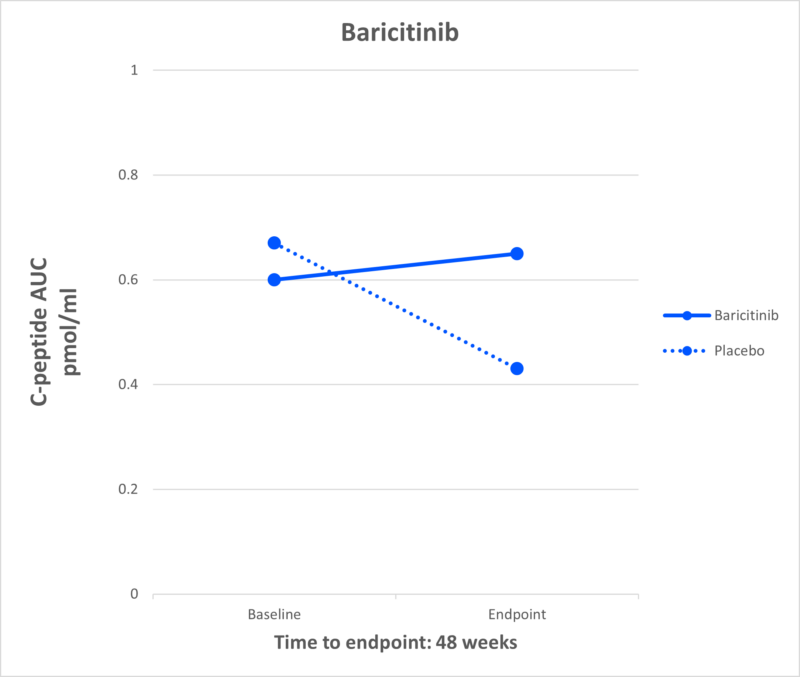
Laura Sanz Villanueva, MSc (St. Vincent’s Institute of Medical Research), who works in the lab of Breakthrough T1D-funded researcher Professor Thomas Kay, MBBS, Ph.D., presented on a mechanistic follow-up study to the BANDIT clinical trial. The Breakthrough T1D-funded phase 2 BANDIT study showed that baricitinib, a JAK1/2 inhibitor that prevents immune cell communication, can increase insulin production as measured by C-peptide in people with recently diagnosed T1D. The present study found that baricitinib can reduce the number of natural killer (NK) cells in the pancreas, which are involved in the autoimmune destruction of beta cells. These data provide valuable insight into the mechanism of baricitinib-mediated protection of beta cells.
Key takeaways
T1D is driven by dysregulation of the immune system, which results in an attack on insulin-producing beta cells. Researchers at ADA 2025 spoked about novel factors—including B cells, NK cells, and T1D autoimmunity triggers—that may contribute to immune cell dysfunction in T1D.
Early detection
A key focus at ADA 2025 was the growing recognition of the heterogeneity of T1D, including autoantibody-negative disease onset, genetic variation, and the frequent misdiagnosis of T1D in adults, underscoring the need for greater diversity and inclusion in research and care. The expanded role of continuous glucose monitoring (CGM) and continuous ketone monitoring (CKM) was also highlighted, not only for daily management but as essential tools for understanding disease progression.
Using genetics to predict T1D risk
- Presenters: Richard Oram, M.D., Ph.D. (University of Exeter), Leslie Lange, Ph.D. (University of Colorado), Aaron Deutsch, M.D. (Massachusetts General Hospital), Josep Mercader, Ph.D.(Massachusetts General Hospital) and Eimear Kenny, Ph.D. (Icahn School of Medicine at Mount Sinai)
- Polygenic risk scores (PRS) estimate the risk a person has for developing a disease like T1D based on variations in different genes.
- Ancestry is a major influence on PRS, particularly based on differences in genes that regulate whether the immune system can distinguish between “self” and “non-self.”
- Most PRS models have been developed using data from European populations and have a limited ability to accurately determine risk in other ethnic groups, such as individuals of African and East Asian descent.
- Potential applications of PRS include incorporation into screening to better understand T1D risk, ensure accuracy in diagnostic tests, and develop precision medicine-based therapeutic approaches.
Understanding how genetic diversity contributes to T1D
- Presenters: Suna Onengut-Gumuscu, Ph.D. (University of Virginia), Dominika A. Michalek, MS (University of Virginia), Aaron Deutsch, M.D. (Massachusetts General Hospital), and Stephen I Stone, M.D. (Washington University School of Medicine), among others.
- These talks highlighted several studies conducted in diverse populations to better understand the pathophysiology of T1D.
- Work presented from Consortia, such as RADIANT, focused on rare and atypical forms of diabetes.
Controversies in CGM and benefits for early detection
- Presenters: Peter Calhoun, Ph.D. (Jaeb Center for Health Research), Michael Kohn, M.D., MPP (University of California San Francisco), Nicole Ehrhardt, M.D. (University of Washington) and Tadej Battelino, M.D., Ph.D. (University of Ljubljana)
- CGM use holds value in identifying progression in early stages of T1D prior to symptomatic onset.
- There was a call to update the clinical guidelines so that the benefits of CGM can be maximized within the T1D community—including at early and later stages of T1D.
- Integrating newer measures of blood glucose, like the glucose management indicator (GMI) and time in tight range (TITR), will be essential.
Contributions of CKM to early detection
- Presenters: Ketan Dhatariya, MBBS, M.D., Ph.D. (Norfolk and Norwich University Hospitals), Lori Laffel, M.D., MPH (Harvard University), Jennifer Sherr, M.D., Ph.D. (Yale University), and Richard Bergenstal, M.D. (HealthPartners Institute).
- It will be critical to explore whether ketone monitoring could help reduce the incidence of diabetic ketoacidosis (DKA) at stage 3 clinical T1D onset.
- Early detection of rising ketones will be important for people with T1D to take action before DKA occurs.
Early detection highlight: Breakthrough T1D-funded research and awardees
Brigitte Frohnert, M.D., Ph.D. (Barbara Davis Center for Diabetes), co-investigator with Breakthrough T1D-funded researcher Andrea Steck, M.D., presented on the evolution of CGM patterns prior to stage 3 T1D. Their longitudinal approach, with CGM data collected at three-month intervals, successfully distinguished individuals who progressed to stage 3 T1D clinical onset from those who did not. This research suggests that CGM may be beneficial for predicting clinical progression of T1D.
Anette-Gabriele Ziegler, M.D. (Helmholtz Munich) was awarded the Harold Hamm Prize for Biomedical Research in Diabetes 2025, highlighting her important contributions on T1D screening in the pediatric population.
Barbara B Kahn, M.D. (Beth Israel Deaconess Medical Center and Harvard Medical School) received the 2025 Albert Renold Award, and her role model for women in science was highlighted at the Women’s Interprofessional Network of the ADA (WIN ADA).
Key takeaways
T1D arises in diverse ways across age groups and ancestries, complicating diagnosis and treatment. At ADA 2025, experts highlighted how genetic and clinical heterogeneity demands more inclusive strategies. Tools like CGM and CKM were highlighted for their potential to enhance clinical management in the early stages of T1D.
Breakthrough T1D’s Cures team making an impact
Sanjoy Dutta, Ph.D., Chief Scientific Officer, participated in a panel discussion titled “Encapsulation vs. Naked Cell Therapy—Immune Challenges and Beta-Cell Perspectives in Diabetes Treatment.” The panelists covered different approaches to preventing immune attack of transplanted islets, including gene-editing, in addition to pros and cons of different transplantation sites.
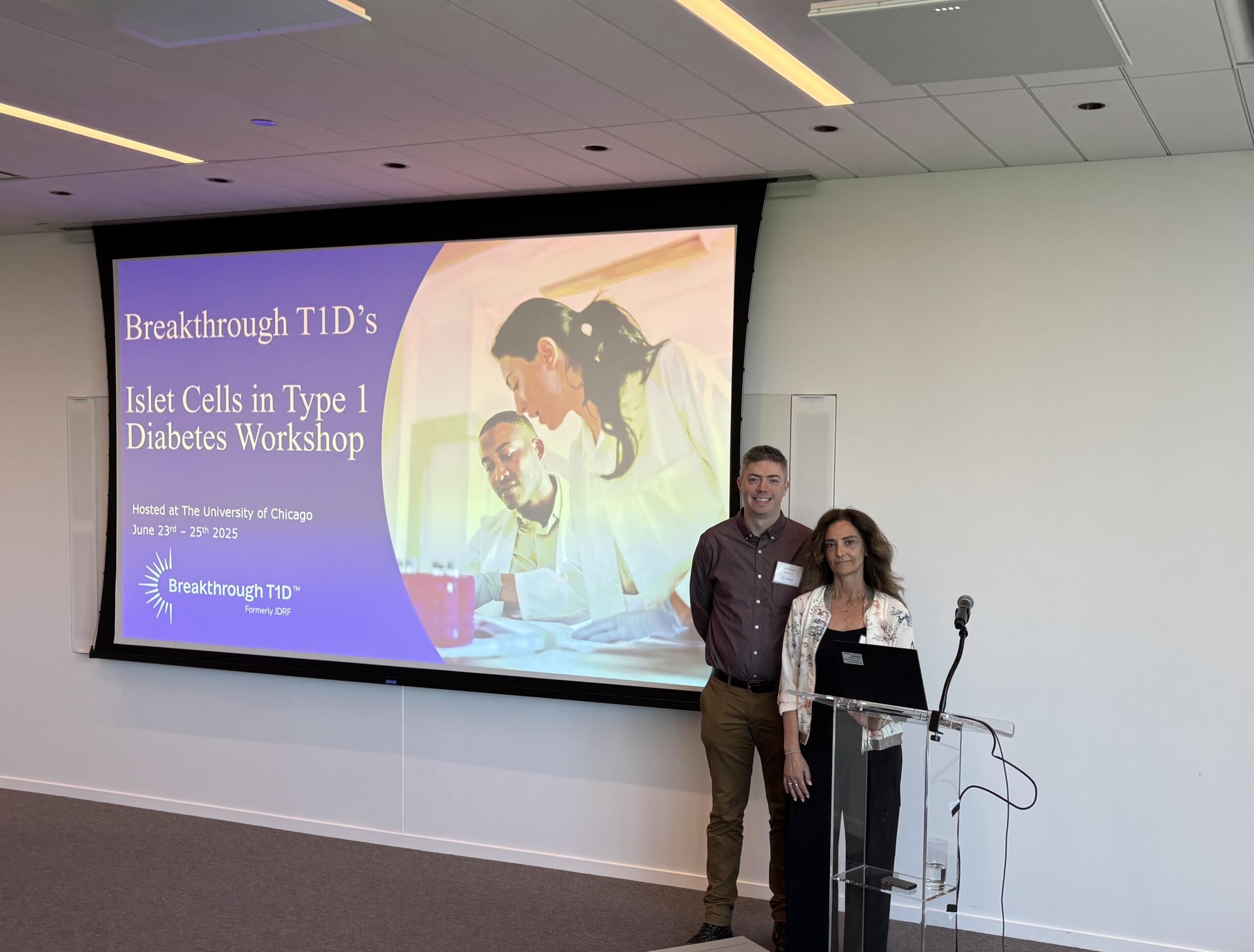
Esther Latres, Ph.D., Vice President of Research, and Jay Tinklepaugh, Ph.D., Senior Scientist, hosted a workshop immediately after ADA titled “Islet Cells in T1D.” Breakthrough T1D-funded researchers gathered from around the world to discuss cell therapy clinical trial updates, mechanistic insights into islet function, targeted delivery of therapeutics to beta cells, and optimization strategies for islet transplantation.
Look out for tomorrow’s article for an update on Medical Affairs presented at ADA 2025!
After months of unexplainable symptoms, Katie Howell was diagnosed with type 1 diabetes (T1D) last year at age 25. Read on to learn more about how she confronted her new reality and became the first participant in New York City to enroll in the DIAGNODE-3 clinical trial.
The unexpected diagnosis

Katie Howell, a Mississippian-turned-New Yorker, has a wide array of hobbies: crafting pottery at her local ceramics studio, enjoying old movies in the theater, cozying up with a book in Prospect Park, and taking in the sun at Rockaway Beach. Katie moved to Brooklyn after completing a Master of Public Administration degree at the University of Tennessee, Chattanooga, and she’s thoroughly enjoying getting to know her new neighborhood.
Suddenly, things took a turn. Last year, Katie started experiencing symptoms of something unknown—for three months, she had no idea what was going on with her body. Then, in a moment of complete shock, 25-year-old Katie was diagnosed with type 1 diabetes (T1D). “Without a family history of T1D and without any health issues of my own, being diagnosed with a sudden, serious chronic illness could not have been more unexpected,” Katie explained.
At the time of her diagnosis, Katie was confronted with a flood of emotions. There was not a single person in her life that had T1D or could understand her experience. “…one of the most challenging parts of being diagnosed with a chronic illness is accepting it […]. This comes with a lot of hopeless feelings, and it is tough to surrender control to an incurable, pervasive, and expensive health condition,” Katie lamented.
Feeling alone and lost, she had no choice but to accept that she was dealing with a major life change—whatever that meant for the future.
Influenced
It wasn’t long before Katie took to social media to learn more about her diagnosis and connect with the T1D community. On Instagram, she stumbled upon Lauren Bongiorno, a T1D influencer. Ms. Bongiorno posted a video promoting DIAGNODE-3, a phase 3 clinical trial for the disease-modifying therapy Diamyd® for early-stage T1D.

Katie found that DIAGNODE-3 was enrolling at The Pediatric Diabetes Center at Hassenfeld Children’s Hospital at NYU Langone. After reaching out to the team at NYU, she realized that the stars had aligned: they had just opened enrollment, and after completing the necessary screening, Katie would be Participant Number One.
“It gets easier every visit!”

Katie received her first study injection in January and will get her third and final injection this month, followed by routine check-ins. This includes blood work, physical exams, and mixed-meal tolerance tests to measure her body’s ability to produce insulin.
As per the study protocol, Katie doesn’t know if she’s receiving the placebo or the study drug, Diamyd®. Still, she likes being in the study: she’s made meaningful connections with the trial team, has learned a lot about T1D, and feels that she’s making a difference—not just for herself, but also for biomedical research.
Katie’s biggest hurdles? Bloodwork and hospitals. “One challenge of this study is the routine blood work and being treated at the hospital. However, it does feel like exposure therapy. It gets easier every visit!” she exclaimed.
Finding her community
Since her diagnosis, Katie has made lasting relationships with others in the T1D community. She connected with the Greater New York Metro Chapter of Breakthrough T1D after volunteering at a Walk in NYC last fall. They introduced her to a group chat with other newly diagnosed young women, where they can ask questions, network, and learn from each other as they navigate their new realities.

“My advice to someone considering [the DIAGNODE-3] trial would be that, though the study is a commitment and an undertaking, they are taking part in discovering medical breakthroughs and T1D treatment research.”
Katie Howell
Participate in clinical trials
Clinical trials are key to bringing medical advancements from the lab to the clinic. This wouldn’t be possible without brave people with T1D, like Katie, who volunteer to participate. These studies offer the potential for life-changing treatment and move the ball forward for the T1D community.
Use our Clinical Trials Matching Tool to find a trial near you. Connect with a Clinical Trial Education Volunteer in your area to learn more about trial participation and answer any questions you may have.

When Tzield was approved by the United States Food and Drug Administration (FDA), the type 1 diabetes (T1D) community had real cause to celebrate: The first disease-modifying therapy for T1D had cleared one of the last major hurdles to becoming available.
Disease-modifying therapies
Also "DMTs" for short, these therapies prevent, slow, halt, or reverse T1D progression.
But once Tzield was on the market and covered by health insurance companies and other payers, a new hurdle emerged: a majority of healthcare providers across the country were unaware of the drug, let alone how to administer it.
The clinical guideline for Tzield infusion did not become available until a year and a half after the FDA approved the drug. To date, 500 people in the U.S. with early stage T1D have received Tzield. Compare that to the annual incidence rate of T1D in the U.S. according to the T1D Index:
According to a 2023 study in the journal Diabetes Technology & Therapeutics, Tzield isn’t the only advanced T1D therapy with a surprisingly low adoption rate.
The FDA approved the first artificial pancreas (AP) system in 2016. Less than a decade later, there are now eight such approved systems on the market. These systems—also called automated insulin delivery (AID) systems—lead to better T1D management and health outcomes—yet only 16 percent of people with T1D in the United States use them.
Similarly, the FDA approved Lantidra, the first donor-derived cell therapy for T1D, in 2023. To date, one person has received it.
Increasing adoption to improve health
Closing the gap between access to and adoption of T1D therapies is a mission priority for Breakthrough T1D.
“It’s similar to the question: ‘If a tree falls in the forest and no one is there, does it make a sound?’” said Anastasia Albanese-O’Neill, Ph.D., APRN, CDCES, Associate Vice President of Breakthrough T1D’s Community Screening and Clinical Trial Education programs. “In this case, if you have a cutting-edge new therapy but most healthcare providers don’t know about it, don’t prescribe it, and don’t know how to administer it, does it have an impact?”
The organization recently announced the establishment of a Medical Affairs unit. The team will address the numerous challenges contributing to the slow adoption of groundbreaking T1D therapies, delaying their life-changing potential for many people living with the disease.
Challenges we are addressing:
HCPs have much greater knowledge of type 2 diabetes—or T2D—which is more prevalent.
HCPs need comprehensive guidelines to support new, approved treatment options.
There are too few clinical environments with the equipment and expertise to administer advanced T1D therapies and treatments, such as new T1D devices, therapies that require infusions like Tzield, and treatments that require implantation, such as cell therapies.
There are too few endocrinologists and certified diabetes care and education specialists with knowledge and competency in advanced T1D therapies.

With the establishment of our Medical Affairs team, we are reaffirming our organization’s commitment to creating a world where every individual with type 1 diabetes has access to life-changing therapies. By addressing systemic barriers and fostering clinical readiness, Breakthrough T1D will be pivotal in driving the timely adoption of emerging therapies and transforming care.”
As part of this organizational change, the Community Screening and Clinical Trial Education team, led by Albanese-O’Neill, will be integrated into Medical Affairs.
The team will focus on developing education materials for healthcare professionals in the U.S. and around the world; empowering people with T1D to participate in shared decision-making with their healthcare teams about emerging T1D therapies; helping to establish and socialize clinical care guidelines tailored to regional needs; and expanding clinical trial participation through community activation and HCP education.
“We have been doing a great deal of work to expand our HCP education, T1D community screening, and clinical trial education programs for more than three years now,” said Albanese-O’Neill, who has been with Breakthrough T1D as a fulltime staff member since 2022. “Given what we are seeing with adoption rates and with Dr. Danne joining us, we are now putting all of this work together in one department with a more strategic approach.”

Empowering clinicians with education
The team recently launched comprehensive, expertly redesigned HCP education and training resources.
These resources—which are accredited, free-of-charge, and live or on-demand—offer a significant focus on early detection for the earliest stages of T1D, monitoring guidance for positive test results, clinical trial opportunities, and the latest on cutting edge T1D therapy research and development, including disease-modifying therapies and islet cell therapies.
While designed specifically for healthcare professionals who can earn 4.5 credit hours of continuing medical education, the resources are available to the public. The on-demand feature means busy healthcare professionals with schedules that include all kinds of shifts imaginable can access this turn-key resource on their own time.
For a deeper dive, Breakthrough T1D’s resources will also offer live sessions, allowing time to interact with and learn from leading experts in the T1D field, including Albanese-O’Neill and Danne, in addition to those affiliated with different clinical facilities and institutions across the nation.

Our goal is to make this education as accessible as possible.”
Detecting T1D before symptoms present
A simple blood test can detect T1D in the earlier stages—before obvious symptoms develop. The biggest challenge is educating clinicians and the general population about it.
“Endocrinologists, Pediatricians, and some other specialty physicians learn about T1D screening and monitoring during their residencies, but it’s not a part of the general curriculum of the first four years of medical school,” said Lally, who built the learning management system for the new resources and is organizing the virtual offerings. “We’re working to advance that knowledge to yes, doctors, but also other clinicians whose patients could benefit.”
Many clinicians hesitate to order unfamiliar tests—especially if they are unsure what to do with the results. Most people who see any kind of healthcare provider could benefit from screening for T1D—according to a paper published in the journal US Endocrinology, roughly 85 percent of people diagnosed with type 1 do not have a blood relative with the autoimmune disease.
“Clinicians need to learn about the stages of type 1 and the specific autoantibody tests that identify type 1 versus type 2 and identifying type 1 in individuals at risk before they need insulin,” said Colleen Buggs-Saxton, M.D. Ph.D.
Buggs-Saxton, a Pediatric Endocrinologist at Wayne Pediatrics in Michigan, is the clinical leader of a Breakthrough T1D Early Detection pilot clinic. Using the new resources, she and Albanese-O’Neill are going to lead a grand rounds about T1D early detection at her institution, which is affiliated with the Wayne State University School of Medicine and healthcare system.

Clinicians should consider autoantibody testing for adults who have been diagnosed with type 2 but don’t have typical clinical features and require insulin to manage their blood sugars.”
“This is a novel way these resources can be used—as the basis of a locally and or virtually-provided grand rounds,” said Albanese-O’Neill.
While much of the emphasis of T1D early detection programs has been on children and teens, its applications are much broader—anyone can develop T1D at any age and unfortunately, misdiagnoses happen. According to an article published in the journal The Lancet, Regional Health: Europe, it is estimated that nearly 40 percent of adults older than age 30 with T1D may have been misdiagnosed with T2D.
“Most clinicians are very comfortable ordering an HbA1c test to classify people with type 2 diabetes, but they do not know what tests to order to classify people with type 1,” added Buggs-Saxton.
Grand rounds
Grand rounds are educational meetings and presentations for clinical teams at a given institution or healthcare facility to provide a summary of updates to the standards of care.

What to do with positive test results
The screening test is just the first part of T1D early detection. Clinicians also need to know what to do with positive results once they come in. Breakthrough T1D’s HCP resources offer extensive education on the topic.
Less than one year ago, Breakthrough T1D and other leading diabetes organizations developed monitoring guidance to help clinicians support people who test positive for stage 1 or stage 2 T1D. The guidelines have been endorsed by leading medical journals and organizations around the world.
”This monitoring guidance can help any clinician feel confident in providing adequate care in the early stages of type 1 and know when to refer to a specialist,” said Albanese-O’Neill.

I think of research, advocacy, and medical affairs as three legs of a stool—in terms of clinical adoption, each helps answer a different question. Research: Does it work? Advocacy: Will the regulators approve it and will insurance companies cover it? Medical Affairs: Do clinical teams have the competency and readiness to prescribe the treatment and educate and support people with T1D?”
It’s also helpful for the people who test positive for early stage T1D. Using the monitoring guidance, people can work with their healthcare team to monitor blood glucose levels to identify when insulin therapy may be needed; consider participating in clinical trials of disease-modifying therapies in development; and consider when and whether Tzield might be appropriate.
“There is currently one FDA-approved disease-modifying therapy for early-stage type 1 diabetes and additional therapies are being studied in clinical trials,” said Lally. “Identifying type 1 early gives the individual and their family time to learn more about type 1 and their options before reaching stage 3 T1D, which requires daily insulin therapy.”

Clinical trials: Increasing patient referrals
Clinical trials are a vital step for any treatment, drug, or device to make it into the hands of people with T1D. Currently, more than 300 clinical trials focused on T1D are actively recruiting participants.
Moreover, clinical trials can offer people the chance of receiving a cutting-edge treatment they may not otherwise be able to access.
Through its HCP resources and existing clinical trial resources, Breakthrough T1D is stressing the significance of investigational T1D therapies—while also clarifying common misconceptions about clinical trials.
“The clinical trial education portion of the program explains current trial opportunities and the critical need to increase diversity in diabetes research,” said Lally.
Despite the importance of clinical trials, many are delayed due to slow enrollment, adding cost and prolonging the results. A 2020 Tufts University study found that nearly 90 percent of clinicians surveyed felt comfortable talking about clinical trials.
“Unfortunately, the survey also revealed that annually, fewer than one percent of patients are referred to clinical trials,” said Lally.
So, why aren’t more clinicians referring their patients to clinical trials? Time and resources.
The most challenging part is helping patients understand what a clinical trial is, what it involves, and how previous scientific advances were only possible because of clinical trials. Healthcare providers often don’t have enough time in their busy clinics to discuss this with patients and families.”
Jacobsen, who is with University of Florida Health (UF Health), is one of the faculty members for Breakthrough T1D’s new HCP resources—specifically, the offering related to currently recruiting clinical trials for T1D disease-modifying therapies.
Jacobsen stresses that families and individuals with T1D also need specific education on the potential of receiving a placebo during a clinical trial—and why it’s an impactful part of any clinical trial.
Clinicians also may not know how to quickly get and stay up to date on current trial opportunities and how to get individuals who test positive for T1D autoantibodies involved.
“We provide a streamlined presentation about how to talk to families of people with T1D or people at risk for T1D about clinical trials,” explains Jacobsen, “We can direct families to one of several websites for more detailed information, like Breakthrough T1D’s Clinical Trial Finder.”

Cell therapies: Cures within reach
Cell therapies are one of the most promising approaches to curing T1D and one of the cornerstones of Breakthrough T1D’s cures research portfolio.
Advances in cell therapies have ramped up in recent years: participants in clinical trials of these therapies have been able to stop taking insulin. To speed this progress even more, Breakthrough T1D recently launched Project ACT (Accelerate Cell Therapies).
Cell Therapies
Also called islet cell therapies, these therapies replace destroyed beta cells so that people with T1D can again produce their own insulin.
The organization has long invested in cell therapy research and has a track record of success in making life-changing T1D therapies a reality—the prime examples being artificial pancreas systems (AP systems) and Tzield.
The work of Breakthrough T1D’s Research, Advocacy, and Medical Affairs teams—in partnership with the organization’s venture philanthropy fund, the T1D Fund—will be integral to Project ACT’s success.
Like AP systems, Tzield, and all other FDA-approved drugs, treatments, and medical devices on the market today, islet cell therapies will only become available after meeting all the required benchmarks—including clinical trials.
Clinicians who are in-the-know about clinical trials and how to help their patients enroll are but one of the numerous ways Breakthrough T1D’s Project ACT will make islet cell therapies a reality, faster.
“Clinicians are generally the most trusted source for this information, but most are not making those referrals, so the gap never closes,” said Lally. “We aim to change that.”
“We want every member of the diverse T1D community to be aware of clinical trials, how to participate, and where to find information,” added Albanese-O’Neill. “The next generation of breakthroughs depends on it.”
Editor’s note: This story co-written by Ginger Vieira, special contributor to Breakthrough T1D.
The “who” of clinical trials
People with type 1 diabetes (T1D) who choose to participate in clinical trials are central to determining whether a new treatment is effective and safe. Yet have you ever wondered who operates behind the scenes of clinical trials?
There are scientists that have researched a new drug or device for years, sometimes decades. There are healthcare professionals (HCPs) that oversee the trial at each location, administer treatments, and monitor participants’ health. There are study coordinators that manage the volunteers. There are pharmacologists, biostatisticians, ethicists, writers, and countless others who analyze and publish the data for the scientific community. It takes a village!
Focus on Hassenfeld Children’s Hospital at NYU Langone
The Pediatric Diabetes Center at Hassenfeld Children’s Hospital at NYU Langone is part of the world-renowned NYU Langone Health system, which also has adult programs for diabetes. Diamyd Medical specifically chose NYU Langone as a trial site for DIAGNODE-3.
DIAGNODE-3 is a Breakthrough T1D-funded phase 3 clinical trial of the disease-modifying therapy Diamyd®. The goal is to preserve as many healthy beta cells as possible to maintain the body’s own insulin production.
The team at Hassenfeld Children’s Hospital managing DIAGNODE-3 is led by Mary Pat Gallagher, MD, the Principal Investigator, Director of the Pediatric Diabetes Center, and associate professor in the Department of Pediatrics at NYU Grossman School of Medicine. With many years of experience under her belt, she has been involved in previous clinical trials for Diamyd®, making her a perfect fit for this final stage of testing.
The team also includes pediatric endocrinologist Dr. Casey Berman, the Sub-Investigator, in addition to Jeniece Ilkowitz, RN, CDCES, and Aashna Shah, who are the study coordinators.
I have a personal and family connection to T1D, and research allows me to have both an impact on the greater community as well as individuals.”
Managing T1D is a team effort—the clinical researchers behind the scenes want to make the process as smooth as possible for those who choose to participate in trials.
“We have a wonderful research team with people who also live with diabetes,” Jeniece continued. “You will receive extra support as you learn to live with your new diagnosis, as we will support you as well as communicate with your primary diabetes provider.”
A deeper dive into the science
Diamyd® is an immune modulator that prevents attack on the body’s insulin-producing beta cells by reprogramming the immune system to ignore GAD (glutamic acid decarboxylase). In T1D, GAD can give rise to autoantibodies, which tell the immune system to destroy beta cells.
This therapy is targeted toward people with newly diagnosed T1D who also have the genetic marker associated with GAD —about 40% of the T1D population.
Diamyd® works by injecting GAD directly into lymph nodes, where immune cells live until they’re needed. If certain types of immune cells are exposed to GAD over and over again, they eventually become tolerant and stop destroying the beta cells.
DIAGNODE-3: The phase 3 trial
Researchers are now testing Diamyd® in phase 3 clinical trials (DIAGNODE-3), the final step before seeking approval from the U.S. Food and Drug Administration (FDA). Results from previous trials have been so promising that Diamyd® has received Fast Track Designation and Orphan Designation from the FDA, solidifying it as a potentially life-changing disease-modifying therapy for newly diagnosed T1D.
To participate in DIAGNODE-3, you must be between 12-28 years old and have been diagnosed with stage 3 T1D within the last six months, meaning you have symptoms associated with high blood sugar and require insulin therapy. You also must test positive for a specific genetic marker (HLA DR3-DQ2) to participate.
Over a two-month period, participants will receive three ultrasound-guided injections into a lymph node located in the groin, followed by a 22-month follow-up. A topical anesthetic can be used as required. While a mild reaction at the injection site (itching, redness, etc.) is expected, to date none of the participants in all the trial phases has discontinued treatment due to injection issues.
For every two participants receiving Diamyd®, one will receive a placebo (a treatment with no therapeutic effect for comparison). Researchers will measure C-peptide, a lab test that shows a person can still produce their own insulin, in addition to HbA1c and continuous glucose monitor (CGM) data to determine whether the drug is working. Based on previous trials, researchers predict that Diamyd® will significantly improve blood glucose management, reduce risk of complications, and overall increase quality of life.
We need your help—get involved!
Clinical trials are critical to get new medicines from the lab into the clinic in a safe and effective way. We know that trials are daunting—signing up to receive a treatment that’s still under investigation can be a difficult decision. Yet, if you choose to participate in a clinical trial, you can have access to new therapies and knowledgeable clinicians, learn more about T1D, and benefit the broader T1D community. Also, because there are only 13 DIAGNODE-3 clinics in the U.S., you may be eligible to receive travel reimbursement.
Meet the team and get screened!
Still feeling unsure? Jeniece, one of the study coordinators at Hassenfeld Children’s Hospital at NYU Langone, suggests starting simple.
“As you wait for the results, you can speak to family and friends with the added knowledge as well as think about your life and how this can fit into it,” she explained. “We truly want to help people living with diabetes and be able to have as many options as possible to help them manage their disease in the future.”
Learn more about DIAGNODE-3 by visiting the study’s website. While there are 60 clinic locations in the U.S. and Europe and more than 200 people with T1D enrolled so far, only one person has enrolled at NYU Langone. If you or anyone you know in the NY Metro Area would be interested in participating, please contact the research team at NYU to learn how to get involved. They are recruiting throughout 2025.
Breakthrough T1D’s role
A pillar of Breakthrough T1D’s Cures Program is disease-modifying therapies: those that can slow, halt, or reverse the course of T1D, such as Diamyd®. These interventions are most impactful at the earlier stages of T1D with the hopes of preserving as many beta cells as possible so that the body can produce its own insulin.
Breakthrough T1D’s funding of the DIAGNODE-3 clinical trial aligns with our dedication to early detection and screening. Identifying the presence of T1D autoantibodies as early as possible allows for a larger window of intervention and increases the chances of preserving healthy beta cells with disease-modifying therapies. While DIAGNODE-3 is the first therapy to target a specific genetic subpopulation of T1D, we anticipate that it won’t be the last, which underscores the importance of getting screened to understand your genetic T1D background.
DIAGNODE-3 is just one of the many different clinical trials that Breakthrough T1D funds.
To promote education and awareness of clinical trials, Breakthrough T1D has assembled a group of Clinical Trial Education Volunteers (CTEVs) who engage with the T1D community.

One CTEV, Alecia Wesner, used her expertise and personal experience with T1D to connect Diamyd Medical, the NYU Pediatric Diabetes Center, the Breakthrough T1D NY Metro Chapter, and Breakthrough T1D National, bringing together critical players who can facilitate participation and spread the word about the DIAGNODE-3 clinical trial.
Without people like Alecia, getting the message out about potentially life-changing trials would be far more difficult. We thank Alecia for her efforts and the clinical trial participants of the T1D community for moving science forward for the benefit of all.
While we look back on 2024, we can reflect upon the incredible progress we’ve made in advancing breakthroughs toward cures and improving everyday life with T1D.
This wouldn’t have been possible without each and every one of you and your continued support of our mission as we drive toward cures for T1D.
Here are the top 11 advances that together, we made happen in 2024:
Breakthrough T1D announced the launch of Project ACT, an initiative aimed at accelerating breakthroughs in T1D cell replacement therapies that do not require broad immunosuppression. Recent advances, such as Vertex’s stem cell-derived islets, have been made possible by Breakthrough T1D’s Cell Therapies program as part of our drive toward cures. The goal of Project ACT is to push research, development, regulatory policies, access, and adoption to increase the rate at which cell therapies without the need for broad immunosuppressants will become available to people with T1D.
Why this matters: Immunosuppressive drugs are a barrier to access to cell replacement therapies because of their toxic side effects, which is why islet transplants are currently only available to people with severe low blood sugar (hypoglycemic) unawareness and episodes. By striving toward a future where we realize the benefits of cell replacement therapies without the downsides of the current regimen of immunosuppressants, we will make islet replacement therapies broadly accessible to the T1D community.
Vertex’s clinical trial of VX-880, a first-generation stem cell-derived islet replacement therapy for people with severe hypoglycemia (requiring the use of immunosuppressants), has transitioned into a phase 1/2/3, or pivotal, trial. This news comes after Vertex shared incredibly promising data in the earlier phases of the trial, including 11 of 12 participants reducing or eliminating the need for external insulin.
The upcoming trial will expand to 50 people who will get a single, target dose of VX-880. The primary endpoint will be insulin therapy independence without severe hypoglycemic events after one year. This is the final clinical testing stage before Vertex can seek FDA approval.
Breakthrough T1D has a decades-long relationship with Vertex and the leading scientists behind stem cell-derived islet therapies, an advancement that would not have been possible without Breakthrough T1D funding and support. The T1D Fund had invested in Semma Therapeutics, which was acquired by Vertex Pharmaceuticals in 2019, eventually leading to the active clinical development of VX-880 in T1D.
Why this matters: This is the first time a scalable cure for T1D is entering phase 3 clinical trials—a significant win and a huge step toward accelerating the delivery of cell therapies to members of the T1D community!
Tegoprubart: Transplant Survival Without Standard Immunosuppressive Drugs
Tegoprubart, an anti-CD40L immunotherapy that limits the immune response, is being tested in a Breakthrough T1D-funded study in people with T1D and severe hypoglycemia who have received deceased donor islets. Eledon Pharmaceuticals announced promising initial results in which two of three people achieved insulin therapy independence. According to the study, tegoprubart is safer for both people and transplanted cells in comparison to broad immunosuppressants, with milder side effects and greater islet survival. To further support this effort, the T1D Fund: A Breakthrough T1D Venture invested in Eledon.
Cell Pouch: A Home for Transplanted Islets
Breakthrough T1D has been supporting the development of Cell Pouch, an implantable device from Sernova that provides a safe, immune-protected environment for transplanted islet cells. In phase 1/2 clinical trials, all six people who received donor islets within the Cell Pouch achieved sustained insulin therapy independence with immunosuppressants, including long-term islet survival and function over five years without harmful side effects.
Why this matters: Standard of care immunosuppressive drugs that help avoid transplant rejection come with unwelcome side effects, such as increased risk of infection and malignancy and toxicity to kidneys, nerves, and islet cells themselves. Breakthrough T1D is focused on finding alternative ways to keep transplanted islet cells alive and healthy so that cell replacement therapies can become more tolerable and accessible.
In a major effort spearheaded by Breakthrough T1D, the first internationally recognized clinical guidelines for those who test positive for T1D autoantibodies have been published. These include guidance on monitoring frequency, education, and psychosocial support in addition to recommended actions for healthcare professionals (HCPs) when the risk of T1D progression is high. The guidelines were cooperatively developed with over 60 international experts spanning ten countries.
Why this matters: Previously, there had been no consensus on monitoring guidelines for people who test positive for T1D autoantibodies. Standardization of clinical recommendations means that individuals, families, and HCPs have tangible next steps to monitor early T1D progression and catch life-threatening complications sooner.
- Breakthrough T1D is leading a campaign to secure a recommendation for T1D screening from the U.S. Preventative Services Task Force (USPSTF), the main authority for preventative care. Approval would require T1D screening to be covered by insurance—an important step forward in expanding access.
- Driven by Breakthrough T1D’s advocacy efforts, The Centers for Medicare and Medicaid Services (CMS) established a unique ICD-10 code for stage 2 T1D. ICD-10 codes are used by HCPs to classify and document diagnoses, symptoms, and procedures. These codes provide a unified way for doctors and providers to indicate what diseases or conditions a person has in their electronic health record (EHR), empowering HCPs to document accurate diagnoses and provide the best possible care.
Why this matters: T1D early detection is critically important to prevent life-threatening complications at diagnosis and to give people necessary resources to make informed decisions about their health. Integrating T1D screening into the U.S. healthcare system will increase access to care.
The past year has seen some important advances in glucose management therapies and devices:
- Cadisegliatin, an activator of a blood sugar regulator in the liver, is being investigated in a phase 3 clinical trial (TTP399) as an adjunct therapy to insulin for people with T1D, although it is currently placed on clinical hold. vTv Therapeutics, the trial sponsor, is also a T1D portfolio company.
- The Omnipod 5 app is now available for the iPhone, making it easier to control the Omnipod without the need to carry a controller. It can also integrate with the Dexcom G6 continuous glucose monitor (CGM).
- Eversense 365 is the first FDA-approved year-round sensor that can easily integrate with automated insulin delivery (AID) systems. Other sensors require replacement after 10-14 days.
Why this matters: While advancements in glucose management have been pivotal in improving health outcomes for people with T1D, access remains a challenge. AID systems are globally underutilized, and not everyone has the necessary technology to connect devices. Breakthrough T1D is working to not only support advances in glucose management but also increase access.
Related content: While Breakthrough T1D consistently strives to improve the lives of those living with T1D, as an organization we have made incredible progress in the development of AID systems, also called the artificial pancreas systems. Read a historical perspective written by Breakthrough T1D volunteer Doug Lowenstein that covers conception to FDA approval of the first artificial pancreas systems, which changed the lives of people with T1D.
An inquiry spearheaded by the Breakthrough T1D affiliates in the U.K. uncovered risks of developing T1D eating disorders (T1DE), including bulimia, anorexia, or insulin restriction to lose weight. There is a significant gap in education and clinical guidelines for HCPs, a lack of internationally recognized criteria for T1DE diagnosis, and insufficient care integration, leading to preventable complications and healthy years of life lost. Breakthrough T1D recognizes the importance of spreading awareness and support for T1DE, and much work is needed to improve the lives of those living with T1DE.
Why this matters: There is an urgent need to change the way T1DE is approached, including integrated physical care with mental health services to get people with T1DE the access to care that they need.
In a study that included people with T1D, finerenone (Kerendia®) has been shown to improve cardiovascular outcomes in adults with heart failure. The drug is already approved in the U.S. to treat kidney and cardiovascular disease in people with T2D. Based on these results, Breakthrough T1D is supporting a clinical trial (FINE-ONE) in conjunction with Bayer to investigate the use of finerenone for T1D with the hopes of reducing kidney complications.
Why this matters: Kidney and cardiovascular disease remain significant challenges for those with T1D, especially given the FDA’s recent rejection of an SGLT inhibitor to lower blood glucose in people with T1D and chronic kidney disease. Yet, a new clinical trial (SUGARNSALT) will better assess the benefits versus risks.
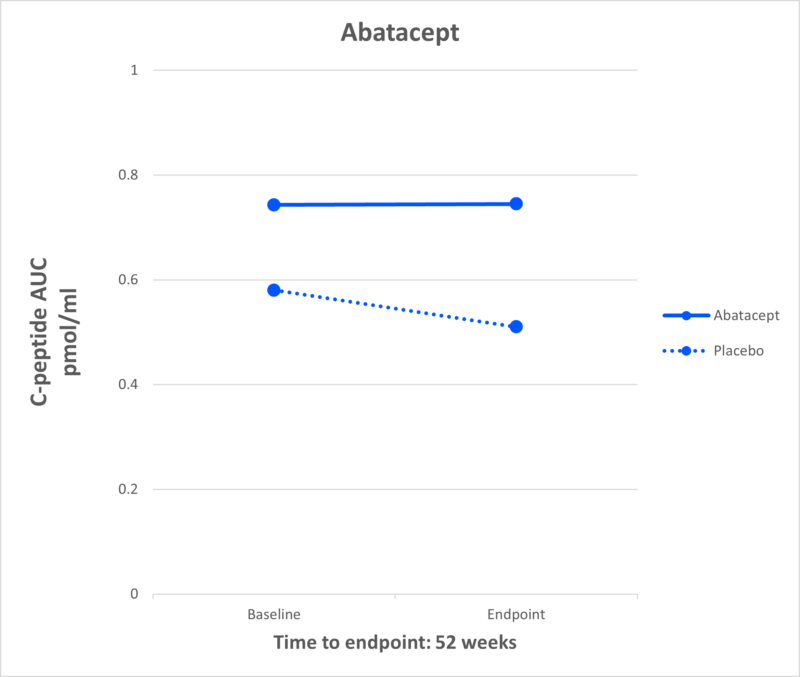
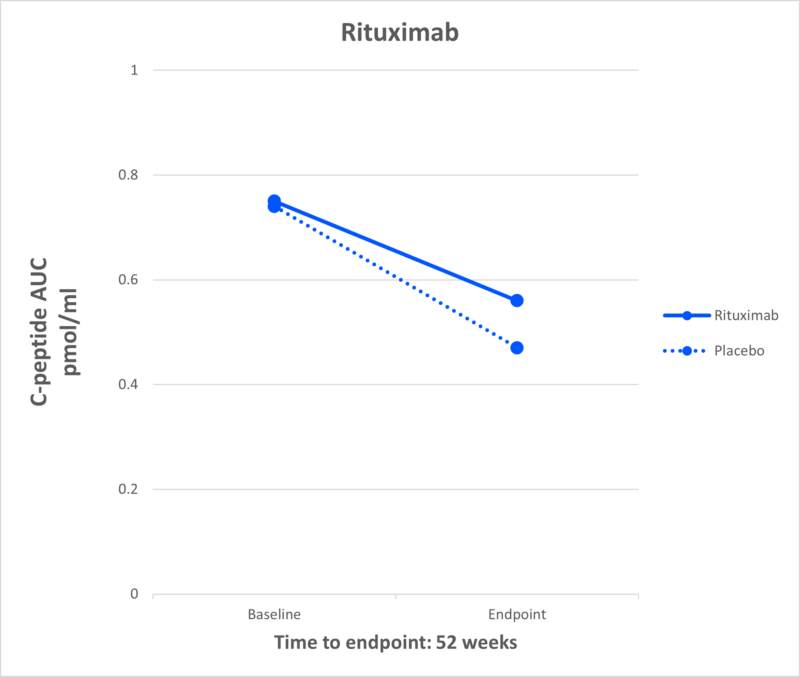
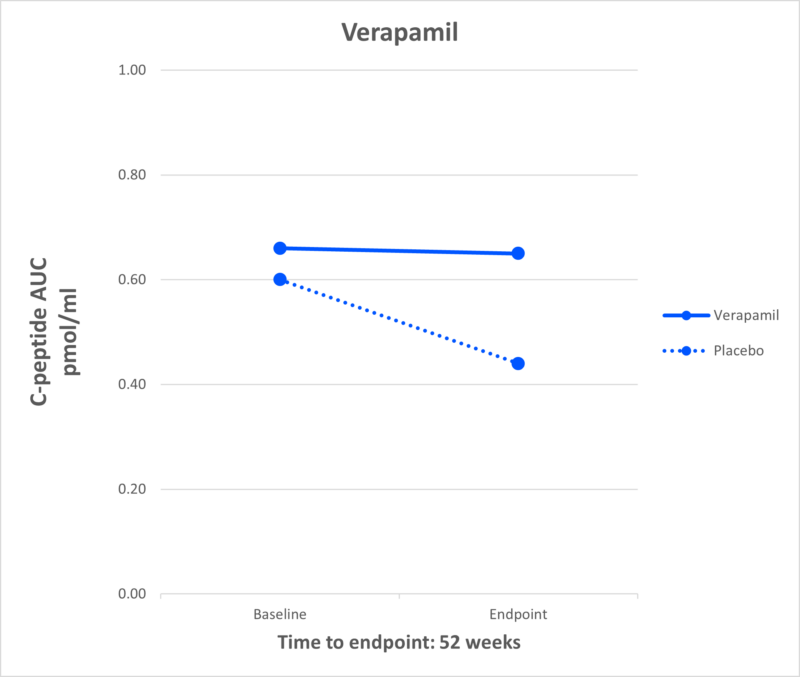
Breakthrough T1D is advocating for the regulatory approval of C-peptide, a biomarker for insulin production by beta cells, to be used as an endpoint in clinical trials. An endpoint can accurately predict a meaningful benefit in clinical trials for disease-modifying therapies (DMTs; treatments that can slow, halt, or reverse T1D). To support this endeavor, Breakthrough T1D scientists and an expert consensus panel published research with evidence supporting C-peptide as an endpoint. Breakthrough T1D is continuing to engage with regulators, coordinate with industry, and assess more clinical trial data to drive this effort forward.
Why this matters: Current clinical trial endpoints (HbA1c, hypoglycemia, and complications) are not the best way to gauge the clinical benefits of T1D therapies. If C-peptide gets regulatory approval to be used as an endpoint, clinical trials could be smaller and shorter while still accurately assessing the advantages of a DMT. This means that drug development can move more quickly, and people with T1D will be able to access therapies sooner.
Related content: Two years ago, the T1D community received the incredible news that Tzield® had become the first FDA-approved disease-modifying therapy that can significantly delay T1D onset. Breakthrough T1D volunteer Doug Lowenstein recounts the life-changing drug’s journey nearly 100 years after the discovery of insulin.
The T1D Index is a data simulation tool that measures the global health impact of T1D, bridging gaps in our knowledge of public health statistics. T1D Index 2.0 has new and improved functionality, including advanced simulation capabilities, validation of data, and enhanced user experience. Breakthrough T1D contributed to both the development and improvement of the T1D Index.
Why this matters: The T1D index is critical in defining the intercontinental scope of T1D, driving us toward country-specific solutions and improved global health outcomes.
Earlier this year, JDRF rebranded to Breakthrough T1D. While our mission remains the same, our name needs to better reflect who we are and where we’re going. Our new brand aligns with our mission to accelerate life-changing breakthroughs for those of every age living with T1D as we work toward a world without it.
Why this matters: The proof is in the name—each day we strive to increase and accelerate breakthroughs in T1D, and it’s critical for our brand to accurately reflect our mission.
It’s certainly been an exciting year! While we still have more work to do, it’s crucial to celebrate our wins, both big and small, to see how far we’ve come in our push to make T1D a thing of the past.
Together, we’re accelerating breakthroughs for people with T1D, and the support of the T1D community drives our mission forward every single day, leading the way to lifechanging therapies and cures. Let’s see what 2025 has in store!
At the 2024 International Society for Pediatric and Adolescent Diabetes (ISPAD) Conference in Lisbon, Portugal, the world’s leading diabetes researchers, academics, and members of industry gathered to share the latest and greatest in diabetes research. Breakthrough T1D leaders and many of our funded researchers and collaborators were on hand —for ISPAD’s 50th birthday—to share new science, breakthroughs, and a glimpse at what the next generation of T1D therapies will look like.
Let’s look at a few highlights!
The T1D Index Levels Up

Breakthrough T1D Chief Scientific Officer Sanjoy Dutta, Ph.D., and Thomas Danne, MD, Chief Medical Officer, International presented a much-awaited update on the T1D Index at ISPAD.
The T1D Index is a first-of-its-kind data simulation tool that measures the human and public health impact of the T1D crisis in every country across the globe. Until the creation of the Index, there have been wide gaps in the data about the incidence and impact of T1D. Leveraging data and insights from the T1D Index can help change the lives of people living with T1D by identifying attainable country-by-country interventions, including timely diagnosis, accessible care, and funding research that could lead to cures.
First , Dr. Dutta gave a refresher on our recent brand evolution, which includes why this change was necessary and how our research strategy has not changed.
Dr. Danne followed with a reintroduction of the Index, its place in our mission, and how we improved it. This includes:
- An enhanced dashboard and user interface designed to improve user experience
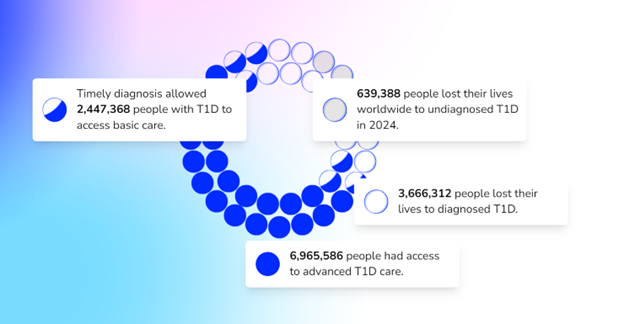
- A plan to develop Index 2.0
- An invitation and plea for all countries and existing registries to collaborate with data to enhance and develop Index 2.0
- Advanced simulation capabilities allowing for scenario analysis.
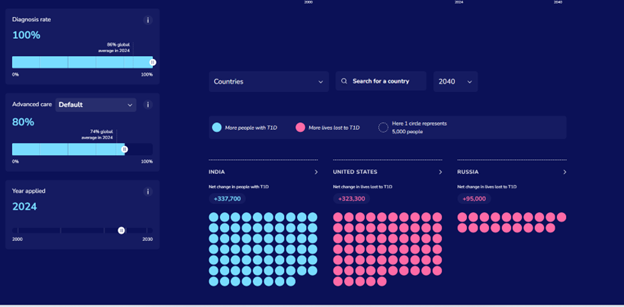
- Validation of data against available national registry data.
- Performance upgrades, including improved platform speed and minor adjustments to further refine accuracy.
In the future, the Index aims to have even more detailed data on a regional level.
Key takeaway:
Breakthrough T1D is focused on improving the lives of people with T1D all around the world—that includes every country in the world. The Index is key to defining the global scope of T1D and the country-by-country solutions to bring better outcomes to everyone affected by T1D.
Is metabolic control enough for young people with T1D?
We have known for decades that T1D is accompanied by the risk of developing complications. The conditions that are most associated with T1D include diabetic eye disease (retinopathy), kidney disease (nephropathy), and heart disease (cardiovascular disease). This is not an exhaustive list—there are many others, including mental health disorders. These complications most commonly occur in adults living with T1D, but new research suggests there’s more we can do to monitor and intervene with these complications in youths with T1D in addition to striving for ideal glycemic control.
At ISPAD, Breakthrough T1D-funded researcher Risa Wolf, MD, discussed long-term microvascular and macrovascular complications in T1D, including the complications mentioned above, and the data is striking. There is a low percentage of complications 4-7 years after diagnosis but after 12 years:
- 24% will have a decline in eGFR (a biomarker for kidney function)
- 13% will have neuropathy
- 52% will have retinopathy
- 28% will have dyslipidemia (abnormal levels of lipids in the blood)
Thankfully, leaps in care management, including automated insulin delivery systems and continuous glucose monitors, have led to improvements in A1c and, in turn, the rate at which people develop complications. But more can be done.
Through regular screening for these more common complications for all youths with T1D, we can better identify, diagnose, and monitor individuals as they develop these complications—especially because many of these screenings are low-cost.
Breakthrough T1D, for example, is funding Dr. Wolf to use the autonomous AI system (IDx-DR, Digital Diagnostics), which is FDA-approved for adults 21+ to detect and diagnose diabetic retinopathy in children. Ideally, this will lead to FDA approval and a better tool for monitoring this complication in kids.
Drs. M. Loredana Marcovecchio – another Breakthrough T1D funded investigator and Didac Mauricio took a similar look at vascular complications. Their presentations had related themes—it is critical to develop ways to identify complications like cardiovascular disease earlier. If they’re identified earlier, individuals can take advantage of the approved therapies.
Key Takeaway:
Like most areas of T1D management: there are still significant unmet needs.
We need to have a long view of these complications and their pathogenesis, which can start in youth. Glycemic control is critical to preventing the onset of these complications, but it is not always enough. Cardiovascular disease, retinopathy, dyslipidemia, and more can all be detected at a young age, which gives more time for interventions.
Breakthrough T1D is working on all of this in our Improving Lives program.
ISPAD / Breakthrough T1D Sessions
Breakthrough T1D Chief Scientific Officer Sanjoy Dutta, Ph.D. joined several collaborators for two sessions.
In the first, titled “Joint-Symposium Breakthrough T1D (formerly JDRF)-ISPAD: Type 1 Diabetes (T1D) Treatments: Hope and Promise Ahead,” two recipients of ISPAD/Breakthrough T1D fellowships, which allow care providers to travel to and receive training at world-class diabetes centers, shared their experiences and how the fellowship enabled them to improve the care they can provide to their communities.
After a presentation from Chantal Matthieu, a longtime Breakthrough T1D investigator, partner and reviewer, Dr. Dutta presented an overview of our work, our vision, and how the next generation of researchers in the room can apply for funding and join us in our work.
In the second session, the Joint ISPAD – Breakthrough T1D symposium, Dr. Dutta and others provided an update on our progress in treating this disease and what’s on the horizon. They touched on the many ways we can slow down disease progression, the exciting state of stem cell-derived cell therapies (they’re in human clinical trials and they’re producing insulin), and how artificial intelligence can play a role in reducing or eliminating T1D misdiagnosis in adults which can be as high as 40%.
Key takeaway:
It’s an exciting time in T1D research, and Breakthrough T1D’s strategy has mapped out what it takes to get to cures—including the importance of bringing in the next generation of researchers to contribute.
Revolutionizing Diabetes Care: Cutting-Edge Therapies
This session, which was a personal favorite of the author, gave updates on the biggest priorities we have at Breakthrough T1D: cures and how close we are to realizing them.
Spoiler alert: we’re not that far away.
It featured presentations from several Breakthrough T1D-funded researchers, including Colin Dayan, MD, Lori Laffel, MD, and Kimberly Simmons, MD.
First up: Dr. Simmons spoke about Tzield, the first disease-modifying therapy approved for T1D, and its use in the real world. A quick summary of the data:
- 322 people have received the drug to date
- The side effects reported in the clinical trial are consistent with what has been seen at the Barbara Davis center
- “Most of our patients have told us that they would do this treatment again.”
- Long term data for how people are tolerating the therapy and progression to T1D is not available yet.
As a reminder, Tzield was FDA-approved in November 2022 for individuals with stage 2 T1D to delay onset by an average of two years. Learn more in this comprehensive story on how it came to be and the role Breakthrough T1D played in getting it to market.
Dr. Michael Rickels then explored cell replacement therapies: where we are and where we’re going. His presentation covered the current landscape: We can use cadaveric islets to restore insulin production in people with T1D. However, the requirement for chronic immunosuppression and scarcity of donor islets mean this is not a viable option for the vast majority of people with T1D.
The next step is using an unlimited supply of stem cell-derived islets and discovering methods to keep them safe without the use of chronic immunosuppression, which is consistent with our strategy in this area.
Dr. Rickels also touched on the study that used autologous cells to restore insulin production in a person with T1D.
Lastly, Dr. Colin Dayan gave an update on combination therapies to preserve beta cell function in people with T1D.
Combination therapies utilize several different therapies that work by discrete mechanisms to target a singular problem. An example is tuberculosis or HIV, which both relied on complicated treatments composed of different pills that had to be taken at different times of day but are now treated with singular pills.
As we have shown, there are many drugs that can preserve insulin production. Now we’re learning which drugs can be taken together to preserve that insulin production longer. Dr. Dayan discussed the T1D Plus study (which builds on the Ver-A-T1D trial), which is funded by Breakthrough T1D, JDRF Australia, INNODIA, and the Helmsley Charitable Trust. This study will test several different drug combinations to see their effectiveness, including Tzield, verapamil, antithymocyte globulin (ATG), and golimumab.
Not only will this trial test multiple drugs—the innovative design of the study will speed up the length of the study, shaving years of the time it will take to see what combinations work best.
Key takeaway:
Breakthrough T1D is at the center of cell therapies and disease-modifying therapies. The clinical trials being run in humans today are very exciting and are a glimpse into how this disease could be treated in the not-too-distant future. It’s possible there will be approved combination therapies to slow progression and cell replacement therapies that restore insulin production entirely in the not-too-distant future.
Until next year!
These are just a few highlights from three days of sessions and presentations that cover our entire research portfolio. For example, Dr. Danne presented on the importance of early detection due to its numerous, clearly defined benefits and strategies for identifying these youths with stage 1 and stage 2 T1D. There were also sessions on the impact of AID systems, specific areas of complications, and much, much more.
We’re already looking forward to next year!
It’s early October, which means the Nobel Prizes are being awarded in several categories. These prestigious awards recognize outstanding contributions in Peace, Literature, Physics, Chemistry, Physiology or Medicine, and Economic Sciences. They go to the best and brightest people with the best and brightest ideas.
This year, the prizes recognize work that is, in several ways, connected to Breakthrough T1D and the work we are doing to cure type 1 diabetes (T1D) and improve the lives of those living with it.
microRNAs
The 2024 Nobel Prize in Physiology or Medicine was awarded to Victor Ambros and Gary Ruvkun for the discovery of microRNA and its role in post-transcriptional gene regulation.
But what is it?
The DNA in our body has between 20,000 and 25,000 genes. Our body constantly activates those genes, which allows it to function. For example, there is a gene that tells the beta cells to start creating insulin in response to elevated blood glucose levels.
This is called gene expression—it’s when the body produces something, usually a protein, to do something specific in the body. Gene expression happens when the DNA of a gene is copied to form messenger RNA, or mRNA, which is then turned into a protein that has a unique function. This is orchestrated in a highly tissue-specific manner, creating diverse cell types like muscle, nerve, beta cell, and more.
In 1993, we learned that molecules called microRNAs regulate gene expression. They can hamper or promote it. By measuring the presence of microRNAs and using them as a biomarker, we can learn a lot about what is going on inside the body, what genes are being expressed, and in which cell types.
How does this apply to type 1 diabetes?
Breakthrough T1D is actively funding research into the use of microRNAs to advance our mission. In fact, we are currently funding $2.6 million in grants related to microRNAs. Specifically, we’re exploring their use as biomarkers of disease progression and as a therapeutic target to interfere with the autoimmunity behind T1D.
Biomarkers
Biomarkers are, put very simply, things in the body that can be measured. Pulse, body temperature, and blood pressure are all biomarkers. In T1D, there are a handful used in common parlance: blood glucose level, HbA1c, time-in-range, autoantibody status, and more. We want to validate the use of microRNAs as a biomarker of disease progression.
We know through years of work that early detection has many benefits. This includes being educated on what T1D is, preparing for a potential diagnosis, the ability to benefit from a disease-modifying therapy to delay onset, and preventing potentially life-threatening complications at onset. microRNAs have the potential to increase our understanding of disease progression and identify how quickly a person is progressing.
Type 1 diabetes occurs in stages. Today, biomarkers of progression, like autoantibody status, don’t paint the whole picture. If a person tests positive for 2 autoantibodies, that means they are almost 100% likely to develop T1D at some point—but we don’t know how fast. We can measure blood glucose levels, but that is a single data point for dysglycemia. It doesn’t tell us how healthy the beta cells are.
microRNAs have the potential to paint a much more detailed picture. We are funding research to discover whether we can use microRNAs to learn exactly where a person is in their progression to stage 3 T1D and how quickly it’s happening.
In summary—we believe microRNAs can enhance the predictive value on top of the current biomarkers for T1D. They can be a very useful tool in measuring progression and helping people in stages 1 and 2 of T1D.
microRNAs as a therapeutic target
Type 1 diabetes is an autoimmune disease—a disease where the body’s immune system destroys its own cells. In T1D, the T-cells in the immune system destroy the insulin-producing cells in the pancreas.
Our research into stopping disease progression focuses mainly on two areas: modifying the immune system and modifying the beta cells. microRNAs can potentially help us fix the dysregulation in the immune system, slowing down or halting the autoimmune attack.
Breakthrough T1D-funded researchers discovered that blocking microRNA-146a in mice can prevent the T-cells from damaging the beta cells. Preventing damage to the beta cells prevents T1D from progressing. Our hypothesis: if we can block microRNA-146a, we can slow down or halt disease progression. This specific study is in a pre-clinical setting, and if it goes well, it could move into clinical trials in the near future.
David Baker – Nobel Prize in Chemistry
David Baker, a breakthrough T1D-funded researcher, was awarded half the 2024 Nobel Prize in Chemistry for computational protein design.
Baker’s prize acknowledges his work in discovering a way to create new proteins that have never existed before. These proteins can potentially be used to treat diseases, make new vaccines, and more. A few years ago, we saw a potential application to T1D.
There haven’t been any groundbreaking changes in insulin since the discovery of synthetic insulin in the late 1970’s. Breakthrough T1D wants to change that—and is funding researchers, like David Baker, to figure out what the next generation of insulins can look like.
Baker received two grants from us from 2016-2021 to use a computer model to create new, glucose-responsive insulin (GRI). GRI is insulin that can be administered, exist in the blood stream, and only be active when it is needed. Baker’s grant was one of many projects we are pursuing in GRI. This work continues to this day, and there are even GRIs in human clinical trials.
What’s next?
This year’s Nobel Prizes show that we are focusing on the same things the Nobel Committee is focused on: the best and brightest scientists and the best and brightest research. Hopefully, one day, we’ll see a T1D scientist win a Nobel Prize for curing this disease.
Want to learn more?
Visit our Funded Research page, where you can read about every single grant we fund—including David Baker’s work in GRI and the many grants currently being funded to study microRNAs.
As the leading global type 1 diabetes (T1D) research and advocacy organization, Breakthrough T1D helps make everyday life with the condition better while driving toward cures. We won’t stop until the condition is a thing of the past.
That means powering research to cure, prevent, and better treat T1D and its complications and ensuring that the entire T1D community has access to the tools they need to thrive.
Breakthroughs past, present, and future
For more than 50 years, Breakthrough T1D has played a pivotal role in nearly every major T1D breakthrough—from how HbA1c came to be more than 40 years ago to recent advancements like advanced T1D management devices, such as artificial pancreas (AP)/automated insulin delivery (AID) systems. Our work has also ensured that people have access to these advances.
Let’s have a look at some of the biggest breakthroughs we’ve advanced that are improving lives right now and those that promise to improve lives in the future.
The first disease-modifying therapy for T1D
In 2022, the FDA approved Tzield™ (teplizumab-mzwv) for use in delaying the onset of clinical T1D. This was the first disease-modifying therapy (DMT) for T1D to be approved. These are treatments that can slow, halt, or reverse the course of a condition. It took decades of Breakthrough T1D research for Tzield to reach approval.
Beginning with basic research by Kevan Herold, M.D., in the 1980s to preclinical and early clinical trials to a strategic investment from the T1D Fund: A Breakthrough T1D Venture that brought Provention Bio—the company that launched Tzield—into T1D for the first time, in 2017.

“The story with the clinical use of teplizumab began with a Breakthrough T1D grant to support a trial in patients with new-onset type 1 diabetes more than two decades ago. The success of this initial study planted a seed that led to further studies and support from the NIH.”
Kevan Herold, M.D.
Yale School of Medicine
But there’s a personal story, too.
Andy Drechsler and his wife Moira are the parents of four children; three of them have T1D. They have been involved with Breakthrough T1D since their son was diagnosed at the age of 22 months in 2005.
Andy’s professional life intersected with his personal life when he helped start Provention Bio in 2017.
“Everyone living with T1D provides us with great inspiration. We also appreciate the parents and caregivers of T1Ds. We are so happy to see the improvements in pumps and CGMs for those living with T1D. We are also thrilled to see therapies to delay the onset. Ultimately, we are confident that therapies will allow many to live without T1D someday.”
Andy Drechsler
Board of Directors President
Breakthrough T1D New Jersey Metro and Rockland County Chapter

We are moving ever closer to a world without this disease. Tzield is one gigantic step along the way, and others are right behind it. Read about the other disease-modifying therapies in our pipeline to learn about the drugs that could become the “next Tzield.”
T1D management devices—decades in the making
For 20+ years, Breakthrough T1D spearheaded efforts to develop artificial pancreas (AP) systems—also called automated insulin delivery (AID) systems. We would go on to fund more than 150 grants, including 50+ clinical trials, funded by us and backed by our Artificial Pancreas Consortium, to make the artificial pancreas system a reality.
Thanks to Breakthrough T1D research and advocacy efforts, approximately 15 FDA-approved T1D management devices are on the market today—more than half of them AP systems and the remainder, advanced CGMs and insulin pumps.
Read about the different AID systems that the U.S. Food and Druge Administration has approved in recent years.

“Witnessing the progression of T1D breakthroughs over the years has been nothing short of remarkable. When I first started insulin injections, it was a cumbersome routine, requiring multiple injections a day. Today, thanks to advancements in insulin pump technology, managing T1D has become more streamlined and efficient, improving my quality of life.”
Princess Padmaja Kumari Parmar
Breakthrough T1D Global Ambassador
Early detection empowers families, helps advance research
T1D develops in stages over time. Early detection identifies people who have early-stage T1D, but no symptoms, by a simple blood test. It looks for markers in their blood called autoantibodies. These autoantibodies signal that the body’s immune system is attacking the insulin-producing cells in the pancreas.
Autoantibodies also have value in identifying individuals who would later develop T1D, providing a new staging for presymptomatic T1D. The presence of two or more means that your lifetime risk of getting T1D is nearly 100 percent.
Early detection gives families time to plan and prepare before the onset of the condition, prevents life-threatening complications and hospitalization at the onset of symptoms. Critically, it also identifies at-risk people who can take advantage of preventive therapies—including disease-modifying therapies such as Tzield—or participate in clinical trials for T1D therapies being developed.
NFL Super Bowl Champion Orlando Brown, Jr., knows all too well how dramatically T1D can impact families, as his late father and his younger brother were both diagnosed with T1D.
In his role as Breakthrough T1D ambassador, the Cincinnati Bengals offensive tackle strives to educate people about T1D and the importance of T1D early detection and research. He also uses his platform to advocate for insulin affordability and policies like the Special Diabetes Program (SDP). Last summer, he was one of 10 Celebrity Role Models at Breakthrough T1D Children’s Congress.
Learn about our program, Breakthrough T1D Early Detection.
“The sudden loss of my father to diabetic ketoacidosis and my younger brother’s type 1 diabetes diagnosis at just 11 years old brought us face-to-face with uncertainty and the stigmas surrounding this condition. However, as we learned about diabetes devices and treatments to help manage the disease, we discovered a renewed sense of peace and hope. With more research, we believe we can ultimately end this disease. Knowledge is power and I’m sharing my family’s story to educate and inspire others who are living with type 1 diabetes.”
Orlando Brown, Jr.
NFL Super Bowl Champion
Breakthrough T1D Ambassador

Breakthrough in progress: stem cell-derived replacement therapies
Cell therapies replace beta cells in the bodies of people with T1D so that they can again produce their own insulin.
Biotech powerhouse Vertex Pharmaceuticals is making major headway in its goal of developing stem cell-derived replacement therapies for T1D. This work being advanced by Vertex has been supported by Breakthrough T1D for decades.
Vertex launched its clinical trial of VX-880, a stem cell-derived islet therapy in T1D for individuals with hypoglycemia unawareness, in combination with immunosuppressive therapy to protect the cells from rejection. Several people who have received VX-880 have been able to stop taking insulin.
This work was pioneered by Doug Melton, Ph.D., whose years of Breakthrough T1D-funded research led to successfully transforming stem cells into beta cells in 2014. A catalytic investment from the T1D Fund in Semma Therapeutics—the biotech company Melton founded to develop a stem cell-derived islet therapy for T1D—was followed years later by Vertex acquiring Semma. Vertex also acquired ViaCyte, which like Semma, had received support from Breakthrough T1D and the T1D Fund for its cell therapies research.
See the timeline of Breakthrough T1D’s support of stem cell-derived islet replacement therapies.
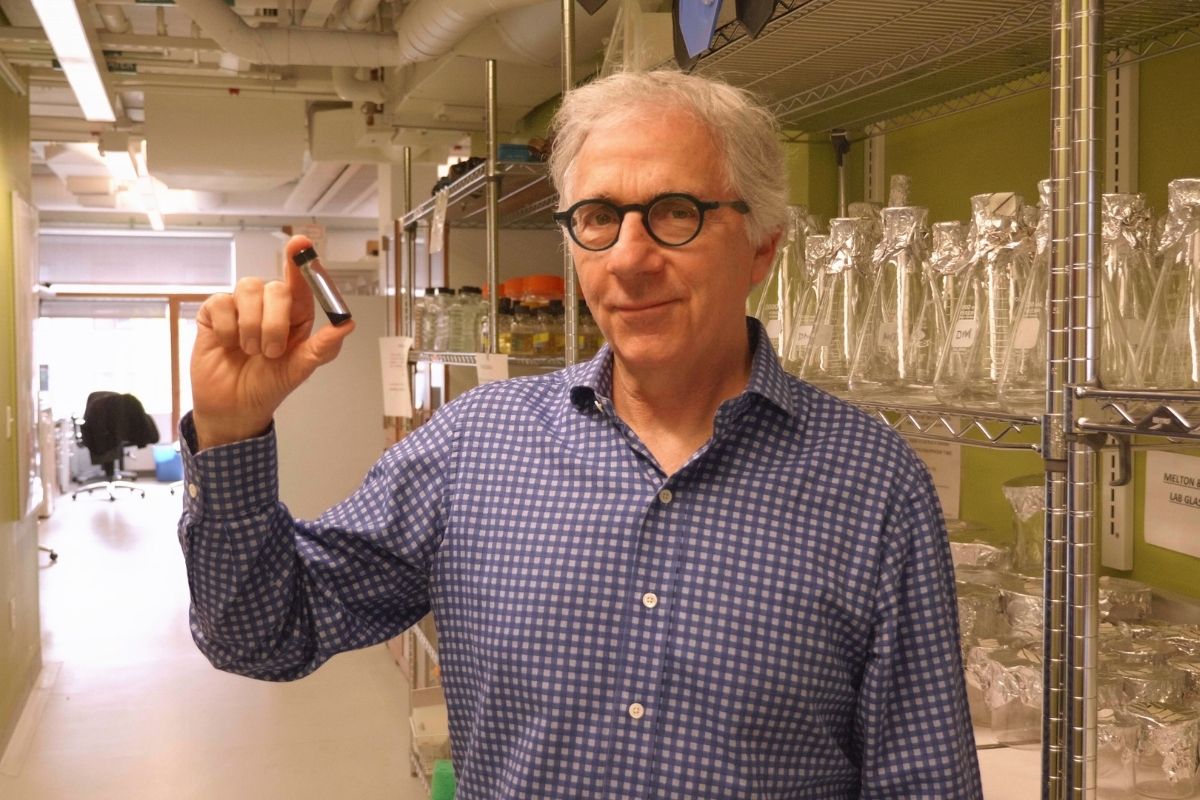
“My lab research has been for more than a decade or two, trying to cure type 1 diabetes. That might sound like an overly ambitious project, but I believe it’s a solvable problem. Our lab worked for years to figure out how to turn stem cells into functional beta cells. We can now make billions of functional beta cells.”
Doug Melton, Ph.D.
Vertex Pharmaceuticals Research Scholar
We are Breakthrough T1D
Breakthrough T1D is knocking on the door of something big. Giant leaps are happening nearly every day. You have gotten us to where we are today—and you can help us get to the finish line faster. So that you, your loved ones, and people everywhere can enjoy a world free from the burden of T1D. A world where people don’t have to manage their diabetes—don’t take insulin, don’t have blood sugar highs and lows, and don’t develop complications. With your ongoing support, we won’t stop until this condition is a thing of the past.
Learn More About Our New Brand.
Learn More About Our Organization.
Last year, Tzield became the first disease-modifying therapy (DMT) approved for type 1 diabetes (T1D). Breakthrough T1D’s disease-modifying therapy pipeline is stocked with other therapies that have the potential to join it as an approved therapy in the US and worldwide.
Disease-modifying therapies are one of, if not the, top success stories of T1D research in 2023. From CLVer to BANDIT to PROTECT, there have been multiple updates on various therapies that can help people with T1D and those at risk for developing it.
This blog highlights eight disease-modifying therapies, including one that is FDA-approved for those at risk for developing type 1 diabetes, their effect in T1D, current research, and more.
Let’s dive in!
What Are Disease-Modifying Therapies?
Disease-modifying therapies are one of the pillars of Breakthrough T1D’s strategy to accelerate the development of cures for T1D.
A disease-modifying therapy is exactly what it sounds like—a therapy that alters the course of a disease. A DMT for T1D is any therapy that slows down the progression of T1D, halts its progression, or reverses it entirely.
Breakthrough T1D is focused on two main tactics to develop DMTs for T1D:
- Stop the immune system from attacking healthy beta cells, preventing T1D from ever occurring.
- Spur beta cell growth safely and protect beta cells, so people with T1D can live without life-long external insulin.
If we can discover a therapy, or combination of therapies that prevent T1D onset and, eventually, reverse it altogether, we will have discovered cures for T1D.
“Type 1 diabetes does not happen all at once—it’s a progression,” said Esther Latres, Ph.D., Breakthrough T1D vice president of research. “For some, the autoimmune process has begun but they are asymptomatic. Others have had T1D for decades and make virtually no insulin. Breakthrough T1D is focused on DMTs that can help everyone with T1D, no matter where they are on the disease continuum.”
The Path Toward Disease-Modifying Therapies
Thanks to decades of Breakthrough T1D-funded work, multiple potential disease-modifying therapies have shown efficacy in altering the course of T1D in people—not just in mice. One of them, Tzield, received FDA approval and is being used in individuals at risk for developing T1D.
There’s also, thanks to Breakthrough T1D and our collaborators, a regulatory pathway for DMTs to receive FDA approval.
Right now, there are multiple disease-modifying therapies approved for other diseases that have shown they can protect and preserve beta cell health in people with T1D.
People who receive these therapies after diagnosis continue to make more of their own insulin, measured by the amount of C-peptide in their blood, than those on placebo. This is a significant finding pointing to the potential application of these therapies to T1D.
According to a new publication made possible by Breakthrough T1D support, “modest concentrations of C-peptide in type 1 diabetes are associated with better clinical outcomes including reductions in hypoglycemia, neuropathy, and retinopathy.” More C-peptide, better outcomes.
Here’s a rundown of several DMTs that, through Breakthrough T1D-funded studies, have the potential to join Tzield as an approved DMT for T1D.
Abatacept
What It Is: Abatacept is a drug that reduces inflammation by inhibiting the activity of the T cells. It is currently approved for use in autoimmune disorders, like rheumatoid arthritis.
Effect in T1D: In 2011, a Breakthrough T1D-funded study showed that individuals receiving abatacept had higher levels of C-peptide compared to placebo.
Current Research: Breakthrough T1D is funding a follow-up study in Australia that uses a nasal insulin as a tolerizing agent to see if using tolerizing agents and immunotherapies at the same time can lead to longer-lasting results.
Breakthrough T1D Role: Breakthrough T1D has supported the development of abatacept for over 15 years and is currently funding a follow-up study.
ATG
What It Is: Anti-thymocyte globulin (ATG) is an FDA-approved drug used to increase white blood cell counts in individuals receiving chemotherapy or transplantation.
Effect in T1D: The Diabetes TrialNet ATG-GCSF New Onset Study found that, after two years, low-dose ATG preserved beta cell function and improved insulin production in individuals newly diagnosed with T1D. People on ATG-alone also had lower A1c levels.
Current Research: There are several Breakthrough T1D-supported studies continuing this research. This includes:
- MELD-ATG – a phase II study conducted by INNODIA, a Breakthrough T1D-supported public/private partnership, to investigate the effect of low-dose ATG on C-peptide at 12 months compared to placebo.
- STOP-T1D – a phase II study conducted by TrialNet, an SDP-funded and Breakthrough T1D-supported network at the forefront of T1D research, investigating if a low dose of ATG can delay or prevent T1D in people ages 12 and up to 35 who have a 50% risk of clinical diagnosis (Stage 3) within 2 years.
Breakthrough T1D Role: Breakthrough T1D has supported the development of ATG for over 10 years and is currently funding follow-up studies.
Baricitinib
What It Is: Baricitinib is a JAK inhibitor currently approved for use in autoimmune disease, including rheumatoid arthritis and alopecia.
Effect in T1D: In a Breakthrough T1D-funded clinical trial published in the renowned New England Journal of Medicine, investigators demonstrated that baricitinib—a JAK inhibitor, which is critical to signaling pathways within both immune cells and beta cells in T1D—preserved beta cell function in the disease.
Current Research: There are several clinical trials to see if JAK inhibitors, like baricitinib, can be effective if used in conjunction with other therapies, such as Tzield or verapamil, in presymptomatic disease, or in longer duration.
Breakthrough T1D Role: Breakthrough T1D, along with Breakthrough T1D Australia, funded the seminal BANDIT study which showed that baricitinib can preserve insulin production in adolescents and teens recently diagnosed with T1D.
Diamyd
What It Is: Diamyd is an antigen-specific immunotherapy, directed toward the autoantigen GAD, to stop the autoimmune destruction of insulin-producing cells. Based upon strong clinical evidence, this therapy is the first to be targeted to a specific T1D sub-population: individuals with the HLA DR3-DQ2 gene, a genetic risk factor for T1D, and presence of antibodies to the GAD antigen. Collectively, this accounts for almost 40% of people with newly diagnosed T1D.
Effect in T1D: In a Phase I/II study, Diamyd demonstrated statistically significant and clinically meaningful beneficial effects on preservation of insulin production and blood glucose control.
Current Research: Diamyd is conducting the DIAGNODE-3 Diabetes Study which will test the safety and efficacy of the therapy in approximately 330 adolescents and young adults aged 12-29 recently diagnosed with T1D.
Breakthrough T1D Role: Breakthrough T1D is funding the DIAGNODE-3 Diabetes study.
Golimumab
What It Is: A monoclonal antibody that inhibits TNF alpha, a chemical messenger that leads to inflammation and increases the immune response to beta cells.
Effect in T1D: Results published in the New England Journal of Medicine in 2020 demonstrated children and adolescents newly diagnosed with T1D who received golimumab produced more insulin compared to placebo.
Current Research: Breakthrough T1D is pursuing this class of drugs to see potential future uses in DMT.
Breakthrough T1D Role: Breakthrough T1D has partnered with other funders to validate the results of this study in combination with another therapy that also preserves C-peptide.
Rituximab
What It Is: Rituximab is a monoclonal antibody medication used to treat certain autoimmune diseases, like rheumatoid arthritis, and types of cancers. It is the only one of the DMTs discussed in this piece that target B cells, the cells that activate the cells that destroy the beta cells.
Effect in T1D: A study by TrialNet showed that rituximab preserved beta cell health in individuals recently diagnosed with T1D.
Current Research: TrialNet is conducting the T1D RELAY study to see if two immune therapies that have shown benefit in T1D—rituximab-pvvr, followed by abatacept—can together preserve insulin production in people recently diagnosed with T1D.
Breakthrough T1D Role: Breakthrough T1D’s work is closely aligned with TrialNet in efforts to develop DMTs for T1D. Breakthrough T1D is currently supporting research into B cells, which is what rituximab targets.
Tzield
What It Is: Tzield (teplizumab-mzwv) is an anti-CD3 monoclonal antibody, FDA approved to delay onset of T1D in at-risk (stage 2) individuals.
Effect in T1D: Tzield delays the progression of T1D by a median of 2.7 years in individuals with multiple autoantibodies and abnormal blood sugar levels. Tzield is the first FDA-approved DMT for T1D.
The results of the PROTECT study, which were recently published in the New England Journal of Medicine, showed that newly-diagnosed individuals can also benefit from this therapy.
Current Research: There are multiple studies, including the Ver-a-T1D trial, to see if Tzield can be used in combination with other therapies to delay T1D progression.
Breakthrough T1D Role: Breakthrough T1D has supported the development of teplizumab for more than 30 years.
Verapamil
What It Is: Verapamil is a generic calcium channel blocker used primarily to treat high blood pressure.
Effect in T1D: Multiple Breakthrough T1D-funded studies, including the CLVer study, have shown that verapamil can preserve beta cells in newly diagnosed individuals.
Current Research: Breakthrough T1D is currently funding a follow-up study for three years to see if C-peptide benefits persist. Additionally, Breakthrough T1D is funding several clinical trials to validate the results of this study and see if verapamil is effective when used in conjunction with other disease-modifying therapies, such as Tzield.
Breakthrough T1D Role: Breakthrough T1D has supported research into verapamil for more than 20 years.
What Comes Next for Disease-Modifying Therapies?
The journey from discovery research to regulatory approval and global access to a drug is long and expensive. Very few therapies make it all the way through because of the vast evidence and resources required.
“Breakthrough T1D wants new therapies to prove safe and effective and get through the regulatory process as efficiently as possible,” said Campbell Hutton, Breakthrough T1D vice president, regulatory and health policy. “We have a team at Breakthrough T1D that works with regulators and industry to ensure this happens. We help establish regulatory pathways, update regulators on the state of T1D science so they are ready to review these new therapies, make sure there is a common understanding of the risks and benefits of new therapies, and more.”
The clinical data reviewed above is critically important for future regulatory approvals. Thanks to dedicated researchers and the contributions of the Breakthrough T1D community, we have significant amounts of data that show the promise of these therapies for people with T1D or at-risk for developing it. However, to achieve regulatory approval, the data, in some cases, will need to be replicated with more people for a longer time.
Even after having the clinical trial data needed, a sponsor, or the company who makes the drug, needs to submit the data and other information, like on the manufacturing of the drug, to FDA (the regulatory agency in the U.S.) for it to be reviewed. If a drug is owned by a single pharmaceutical company, they are responsible for submitting the application as the sponsor. If a drug’s patent has expired and is made by multiple companies, it can be challenging to find a company willing to engage in the long and expensive regulatory process.
Breakthrough T1D plays a key role here, encouraging industry to support clinical research and take the necessary steps to get these therapies to market.
As you can see, this is a complicated process, which is why Breakthrough T1D has filled the pipeline with therapies that all have a decent shot of making it to market.
Breakthrough T1D Enabling Progress in Disease-Modifying Therapies
Breakthrough T1D is the only organization that supports therapy development at every stage—from discovery research all the way through to people with diabetes receiving these therapies—with healthcare coverage paying for them. This is a lengthy and expensive process; success requires many stakeholders to come together toward a common goal. Breakthrough T1D plays a crucial role here to ensure this collaboration happens and everyone, from researchers to regulators to payers—are all pulling in the same direction.
Breakthrough T1D is committed to having multiple shots on goal to cure T1D. The DMT pipeline, as evidenced by the eight DMT candidates above, is proof of that commitment.
Hopefully in the future one of these, or other therapies, will join Tzield and give the T1D community another option for delaying, halting progression, or eventually reversing this disease.
Key Terms to Know
We know type 1 diabetes research has its own language. Here’s a quick refresher on frequently-used terms.
Antibody – blood protein created in response to an antigen
Antigen – something that causes an immune response
Beta cells – cells in the pancreas that produce insulin. These are the cells destroyed by the immune system in people with T1D.
C-peptide – a biomarker that indicates the presence of insulin production. When the body produces insulin, it also creates C-peptide.
HbA1c – a blood test used to measure average blood glucose levels over the past three months.
Immunotherapy – drug aimed at altering the body’s immune system. Specifically, immunotherapies for T1D are intended to disrupt the autoimmune attack behind T1D. Also called “immune therapies.”
Placebo – A treatment, such as a dummy pill, that does not contain any of the drug being tested.